Figures & data
Table 1. Conditions that may be confused as acute stroke (stroke mimics).
Table 2. Clinical characteristics differentiating stroke from mimic.
Figure 2. Patient presented with sudden onset right-sided numbness and no other deficits. Routine computed tomography (CT) was normal. A: Diffusion-weighted (1.5 T) magnetic resonance imaging (DWI-MRI) was normal. B,C: High resolution 3 T MRI (DTI and DWI-isotropic voxels) revealed left thalamus infarction.
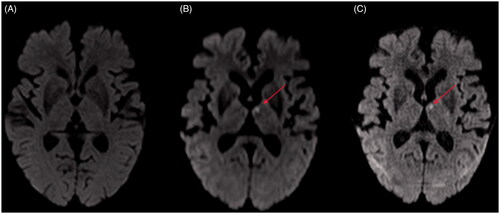
Figure 3. 80-year-old female with atrial fibrillation on apixaban. She presented with a 90-min history of sudden onset right arm and leg weakness sparing the face with normal sensation. A,B: Axial computed tomography (CT) head, CT angiogram (not included) and CT perfusion were unremarkable. Tissue plasminogen activator (tPA) was no given because the patient is on an anticoagulant. C: Diffusion-weighted magnetic resonance imaging (DWI-MRI) was normal. D,E: Sagittal and axial MRI spine revealed right posterolateral epidural haematoma, a multifocal severe spinal canal stenosis, and spinal cord oedema.
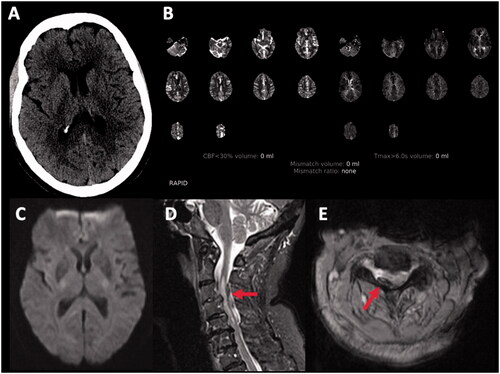
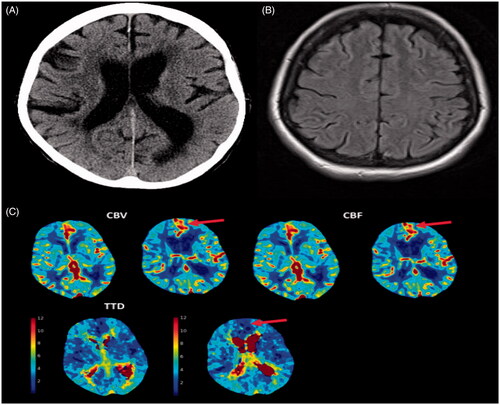
Figure 4. An 85-year-old female presented with expressive aphasia. A,B: Axial computed tomography (CT) head, CT angiogram (not included), magnetic resonance imaging (MRI) of the brain that also included diffusion-weighted imaging were unremarkable. The patient was discharged with the diagnosis of transient ischaemic attack (TIA). After discharge, the patient continued to have recurrent similar episodes. C: CT perfusion during one of her episodes demonstrated left frontal focal hyperperfusion characterized by increased cerebral blood flow (CBF), cerebral blood volume (CBV) and decreased time to drain (TTD). The patient was diagnosed with focal seizure with preserved awareness.