Figures & data
Table 1. Baseline characteristics (N = 4620).
Figure 1. Distribution of clinical and laboratory variables on admission amongst the six COVID-19 subphenotypes. Clinical and laboratory variables on admission normalized and divided into quintiles. Latent class analysis identified six underlying COVID-19 subphenotypes which were notable for varying levels of inflammation, vital sign abnormalities and/or organ dysfunction. T max: maximum temperature; O2 Sat min: minimum oxygen saturation; HR max: maximum heart rate; SBP min: minimum systolic blood pressure; DBP min: minimum diastolic blood pressure; Na: sodium; K: potassium; Ca: calcium; HCO3: bicarbonate; BUN: blood urea nitrogen; Cr: creatinine; BNP: brain natriuretic peptide; WBC: white blood cell count; Hgb: hemoglobin; Plt: platelet count; PT: prothrombin time; PTT: partial thromboplastin time; AST: aspartate aminotransferase; ALT: alanine transaminase; T bili: total bilirubin; IL-6: interleukin 6; IL-1B: interleukin 1B; LDH: lactate dehydrogenase; CRP: c-reactive protein; ESR: erythrocyte sedimentation rate; Procal: procalcitonin.
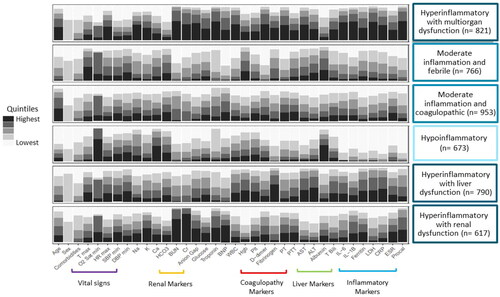
Figure 2. Associations between COVID-19 subphenotype and (A) mortality; (B) intubation; (C) intensive care unit (ICU) admission; and (D) length of stay amongst survivors. Robust Poisson regression to determine the relative risk of outcomes by subphenotype as compared to hypoinflammatory subphenotype where circles represent estimate and bars represent 95% confidence intervals. Multivariable model (shown here) adjusted for onset time, hospital, self-identified race/ethnicity and insurance provider. Hypoinflam.: Hypoinflammatory; Mod inflam. Fever: Moderate inflammation with fever; Hyperinflam. Liver dysfunc.: Hyperinflammatory with liver dysfunction; Mod inflam. Coagulopathy: Moderate inflammation with coagulopathy; Hyperinflam. Renal dysfunc: Hyperinflammatory with renal dysfunction; Hyperinflam. Multiorgan dysfunc.: Hyperinflammatory with multiorgan dysfunction.
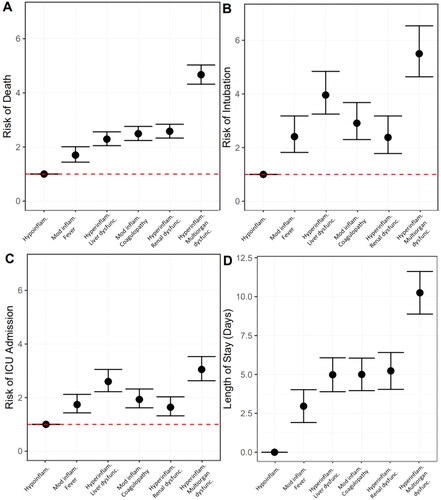
Figure 3. Risk of dying by subphenotype in those who did (blue bars) and did not (red bars) receive convalescent plasma. Robust Poisson regression models adjusted for onset time, hospital, self-identified race/ethnicity and insurance provider stratified by receiving convalescent plasma versus not. P-interaction terms generated by robust Poisson multivariable regression with introduction of an interaction term. P-interaction terms of less than 0.10 are shown. Hypoinflam.: Hypoinflammatory; Mod inflam. Fever: Moderate inflammation with fever; Hyperinflam. Liver dysfunc.: Hyperinflammatory with liver dysfunction; Mod inflam. Coagulopathy: Moderate inflammation with coagulopathy; Hyperinflam. Renal dysfunc: Hyperinflammatory with renal dysfunction; Hyperinflam. Multiorgan dysfunc.: Hyperinflammatory with multiorgan dysfunction. Number at risk per subphenotype (those who received convalescent plasma/those who did not): Hypoinflammatory (2/19), Moderate inflammation, fever (10/82), Hyperinflammatory, liver dysfunction (18/179), Moderate inflammation, coagulopathy (25/253), Hyperinflammatory, renal dysfunction (11/186), Hyperinflammatory multiorgan dysfunction (27/530).
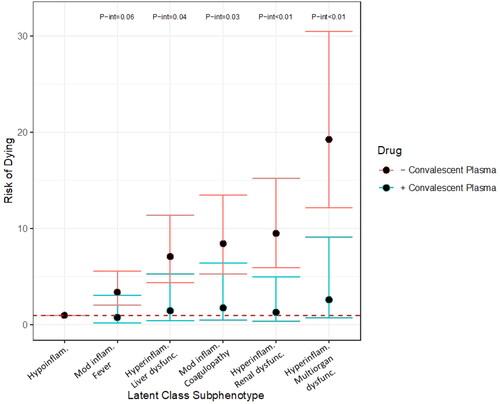
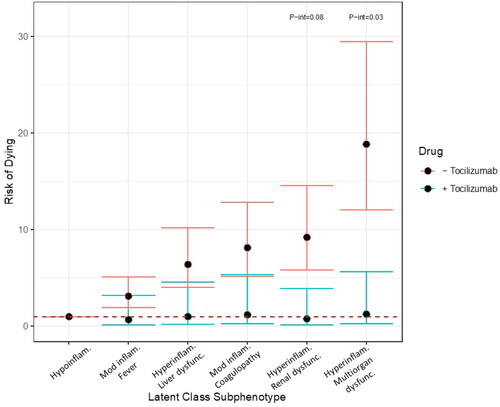
Figure 4. Risk of dying by subphenotype in those who did (blue bars) and did not (red bars) receive tocilizumab. Robust Poisson regression models adjusted for onset time, hospital, self-identified race/ethnicity and insurance provider stratified by receiving tocilizumab versus not. P-interaction terms generated by robust Poisson multivariable regression with introduction of an interaction term. P-interaction terms of less than 0.10 are shown. Hypoinflam.: Hypoinflammatory. Mod inflam. Fever: Moderate inflammation with fever; Hyperinflam. Liver dysfunc.: Hyperinflammatory with liver dysfunction; Mod inflam. Coagulopathy: Moderate inflammation with coagulopathy; Hyperinflam. Renal dysfunc: Hyperinflammatory with renal dysfunction; Hyperinflam. Multiorgan dysfunc.: Hyperinflammatory with multiorgan dysfunction. Number at risk per subphenotype (those who received tocilizumab/those who did not): Hypoinflammatory (1/20), Moderate inflammation, fever (14/78), Hyperinflammatory, liver dysfunction (37/160), Moderate inflammation, coagulopathy (26/252), Hyperinflammatory, renal dysfunction (6/191), Hyperinflammatory multiorgan dysfunction (34/523).
Supplemental Material
Download PDF (185.2 KB)Data availability statement
The deidentified data presented in this study is available upon request from the corresponding author.
