Figures & data
Figure 1 Mechanisms underlying endothelial dysfunction and the functional consequences of decreased vascular bioavailability of nitric oxide(NO). In the presence of cardiovascular risk factors such as hypertension, diabetes mellitus, smoking, age, menopause, familiar history of cardiovascular disease and hypercholesterolemia, vascular superoxide‐producing enzymes such as the vascular NADPH oxidase, the xanthine oxidase (XO), and an uncoupled endothelial nitric oxide synthase (eNOS) produce large amounts of superoxide (O2·−), which will metabolize NO. The consequences are adhesion and infiltration of the vascular wall with inflammatory cells such as macrophages and neutrophils and a subsequent intima proliferation.
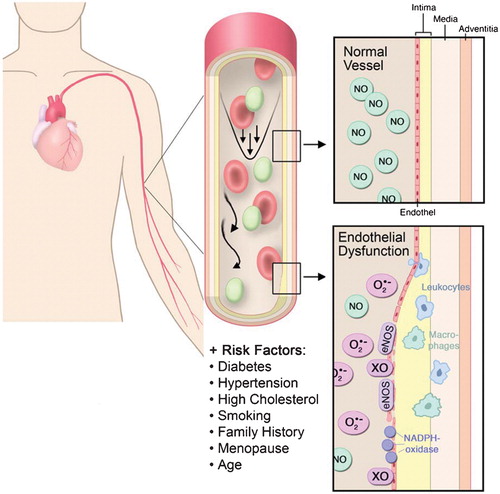
Figure 2 Regulation of vascular tone by the endothelium. The endothelial nitric oxide synthase(eNOS) synthesizes NO by a two‐step oxidation of the amino acid L‐arginine thereby leading to the formation of L‐citrulline. NO is released into the bloodstream thereby inhibiting platelet aggregation and the release of vasoconstricting factors such as serotonin and thromboxane. NO diffuses also into the media and activates the soluble guanylate cyclase (sGC). The resulting second messenger cGMP in turn activates the cGMP‐dependent kinase, which mediates decreases in intracellular Ca2+ concentrations thereby causing vasorelaxation. The physiological stimuli to release NO are shear stress and pulsatile stretch. Intra‐arterial infusion is used in the clinics to assess endothelial function. Infused into the forearm (brachial artery) acetylcholine (ACh) causes a dose‐dependent vasodilation. In the coronary artery the response (vasoconstriction versus vasodilation) strictly depends on the functional integrity of the endothelium. In the presence of cardiovascular risk factors and endothelial dysfunction ACh will cause vasoconstriction due to stimulation of muscarinergic receptors in the media. muscarinic acetylcholine receptor (M), nitroglycerin (NTG).
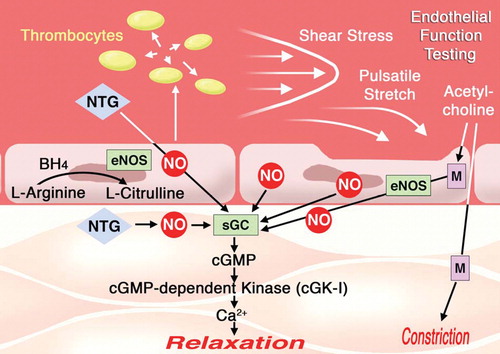
Figure 3 Different invasive and noninvasive methodologies to assess endothelial function in patients with cardiovascular risk factors. A: intracoronary infusion of acetylcholine; B: flow‐mediated dilation; C: forearm plethysmography; D: finger plethysmography. Representative reactive hyperemia peripheral artery tonometry recordings of subjects with normal and abnormal reactive hyperemic response. Normal response is characterized by a distinct increase in the signal amplitude after cuff release compared with baseline. blood pressure (BP), flow mediated dilation (FMD), acetylcholine (ACh), L‐NG‐monomethyl arginine (L‐NMMA).
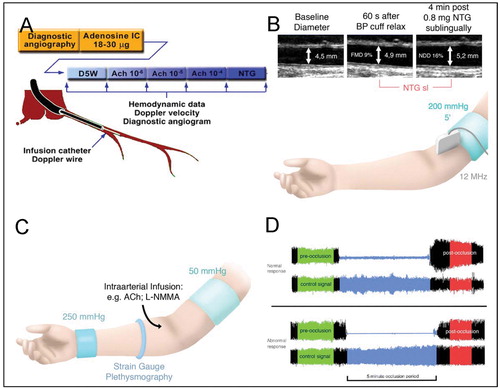
Figure 4 Plots of forearm blood flow to acetylcholine in normal subjects, hypercholesterolemic patients, long‐term smokers, and patients with hypercholesterolemia who smoked. This figure clearly shows the marked potentiation of endothelial dysfunction when two risk factors such as smoking and hypercholesterolemia are present at the same time (adapted from: Heitzer T, Ylä‐Herttuala S, Luoma J, Kurz S, Münzel T, Just H, Olschewski M, Drexler H. Cigarette smoking potentiates endothelial dysfunction of forearm resistance vessels in patients with hypercholesterolemia. Role of oxidized LDL. Circulation. 1996 Apr 1;93(7):1346‐53.)
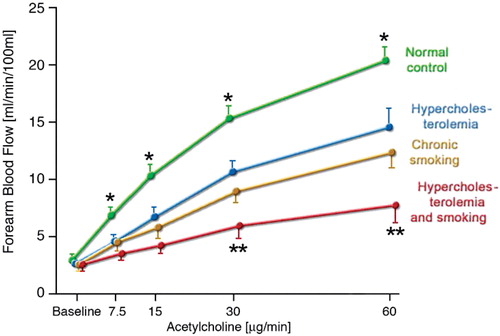
Figure 5 Mechanisms underlying endothelial(vascular) dysfunction in vascular disease. In the presence of risk factors, superoxide‐producing enzymes such as the NADPH oxidase produce large amounts of superoxide (O2·−). Superoxide rapidly reacts with nitric oxide (NO) to form the highly reactive intermediate peroxynitrite (ONOO−). Peroxynitrite causes vascular dysfunction in several ways. It causes tyrosine nitration of the prostacyclin synthase (PGI2‐S) thereby shutting down PGI2 production. Peroxynitrite is also a strong inhibitor of the soluble ganylate cyclase (sGC), thereby inhibiting NO signaling. ONOO− can also oxidize the BH4 to the so‐called BH3· radical. This can decay to BH2 thereby causing eNOS uncoupling. This means that the antiatherosclerotic NO‐producing eNOS is switched to a superoxide‐producing proatherosclerotic enzyme. Vitamin C has been shown to recouple eNOS by reducing the BH3· to BH4 (see insert).
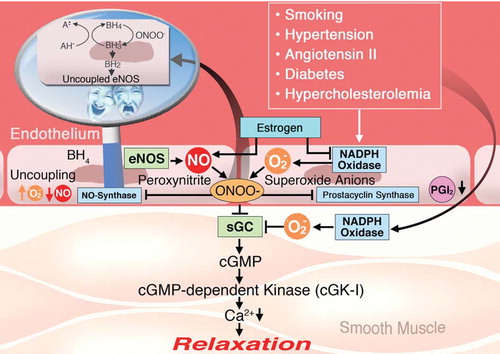
Table I. Biomarkers reflecting endothelial dysfunction (injury).
Figure 6 Chronic oxidative stress causes senescence of endothelial cells. This is characterized by a detachment of endothelial cells or part of the endothelial cell membrane(microparticles; A). B: With the persistence of oxidative stress, the capacity of neighboring endothelial cells to repair endothelial injury is limited, and vascular integrity becomes dependent on the incorporation of endothelial progenitor cells (EPCs) (adapted from Citation87).
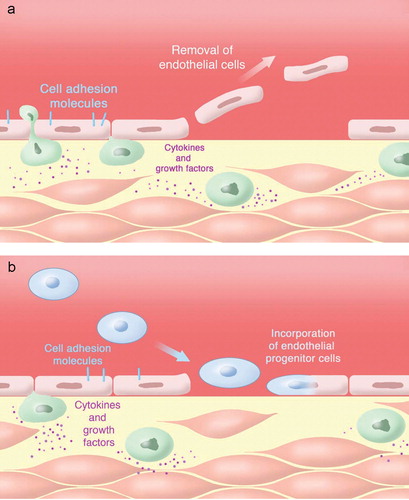
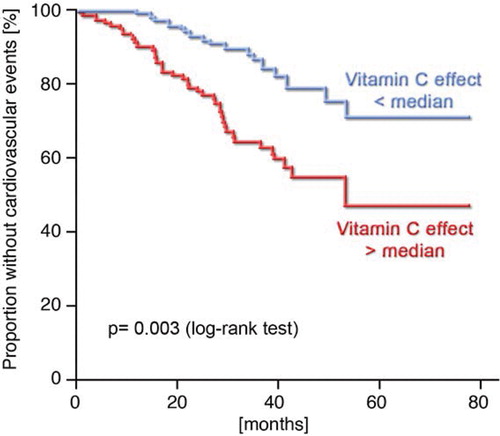
Figure 7 Kaplan‐Meier analysis demonstrating cumulative proportions of patients without cardiovascular events during follow‐up. The figure clearly shows that patients who react strongly to vitamin C with an improvement of endothelial dysfunction have a worse prognosis as compared to patients with a weaker vitamin C response. This means that patients with high oxidative stress in the forearm vasculature may also have more cardiovascular events such as myocardial infarction, death due to myocardial infarction, stroke, and coronary revascularization procedures Citationadapted from Ref. 68.