Figures & data
Figure 1. Incidence (%) of morbid and fatal events in 4 groups of patients divided according to the proportion of the overall treatment duration (<25% to ≥75%) in which blood pressure (BP) was reduced <140/90 mmHg prior to the occurrence of an event. Squares indicate diabetic patients (n = 5250) and circles indicate all patients (n = 15,245). The primary endpoint was a composite of a variety of cardiac morbid and fatal events (see Material and Methods); CV: cardiovascular; MI: myocardial infarction; CHF: congestive heart failure. *All patients without GCP deficiencies and missing BP values.
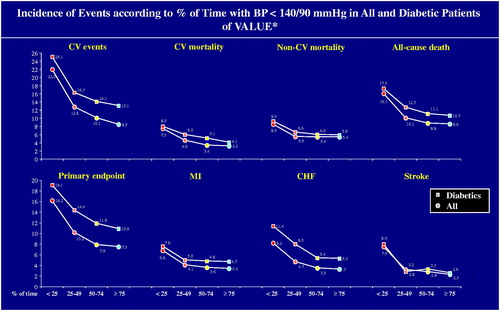
Figure 2. Percent increase taken from Hazard Ratios (HRs) of morbid and fatal events in 4 groups of patients divided according to the proportion of the overall treatment duration (<25% to ≥75%) in which blood pressure (BP) was reduced < 140/90 mmHg prior to the occurrence of an event. Diabetic patients (n = 5250) are compared with all patients (n = 15,245). The groups in which BP was reduced <140/90 mmHg for ≥75% of the time is used as reference and shown by the empty circle. CV: cardiovascular; MI: myocardial infarction; CHF: congestive heart failure; BMI: body mass index; SBP: systolic BP; DBP: diastolic BP; CVD: cardiovascular disease; LVH: left ventricular hypertrophy. *Adjusted for baseline covariates (age/gender/BMI/SBP/DBP/diabetes/CVD history/high cholesterol/LVH/proteinuria). §Statistically significant difference with group with BP <140/90 mmHg ≥75% of the time.
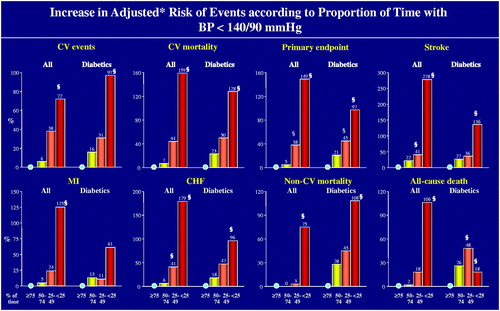
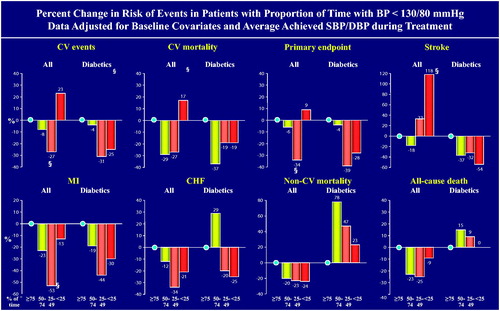
Figure 3. Percent increase taken from Hazard Ratios (HRs) of morbid and fatal events in 4 groups of patients divided according to the proportion of the overall treatment duration (<25% to ≥75%) in which blood pressure (BP) was reduced < 130/80 mmHg prior to the occurrence of an event. Diabetic patients (n = 5250) are compared with all patients (n = 15,245). The groups in which BP was reduced < 130/80 mmHg for ≥75% of the time is used as reference and shown by the empty circle. Calculated HRs were adjusted for baseline covariates, i.e. age, sex, body mass index, history of CV events, diabetes (not diabetes mellitus group), smoking, left ventricular hypertrophy, hypercholesterolaemia, proteinuria, systolic BP and diastolic BP. CV: cardiovascular; MI: myocardial infarction; CHF: congestive heart failure. §Statistically significant difference with group with BP <130/80 mmHg ≥75% of the time.
Online_Supplement_Tables_1-4_DM___ALL_20.11.20.ppt
Download MS Power Point (270 KB)Data availability statement
The data that support the findings of this study are available from the corresponding author, S.E.K. upon dire needs.
