Figures & data
Figure 1. Chronology of the development of beta-blockers. The illustration depicts the pharmacological properties characterising the three “generations” of this development. BP indicates blood pressure and HR indicates heart rate.
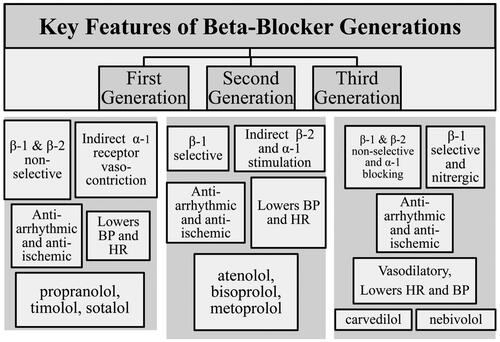
Figure 2. Chemical formulas for the beta-blocker. For some beta-blockers that exist in more than one formula, only one of these is included in this overview. For the function of a beta-blocker, the compound contains an aromatic ring and a β-ethanolamine. The aromatic ring can be either benzo-heterocyclic (such as indole) or heterocyclic (such as thiadiazole). Moving the acyl-amino group to meta- or ortho-positions, on the benzene ring, causes a loss of selectivity but not loss of the β-blockade. This pinpoints the significance of para-substitution for beta-1 selectivity of beta-blockers. Side chains can either be directly linked to the aromatic ring or linked through a —OCH2— group and change the properties of the molecule explaining the intrinsic sympathomimetic (agonist) activity or changing the lipophilic properties. Concomitant alpha-blocking or nitrergic activities and beta-2 agonist activities contribute to vasodilation. Upper left box: Beta-1 selective atenolol (At), betaxolol (Be), bisoprolol (Bi), esmolol (Es), metoprolol (Me), and nebivolol (Ne), which has also nitrergic effects. Lower left box: Beta-1 selective with intrinsic sympatho-mimetic (agonist) activity – celiprolol (Ce, beta-2 agonist), acebutolol (Ac), and xamoterol (Xa). Upper right box: Beta unselective with intrinsic-sympatho-mimetic (agonist) activity – carteolol (Cart), bucindolol (Bu), alprenolol (Al), oxprenolol (O), penbutolol (Pe), and pindolol (Pi). Centre box: alpha and beta-unselective carvedilol (Carv) and labetalol (La). Lower right box: non-selective nadolol (Na), propranolol (Pr), sotalol (So) and timolol (Ti).
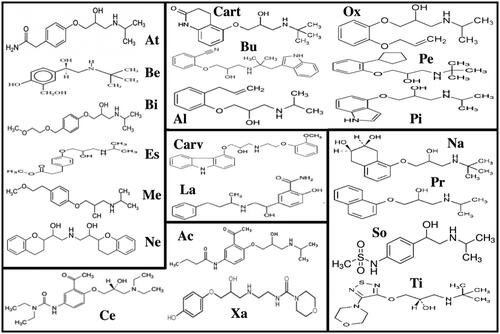
Figure 3. Diversity of the beta-blockers. Beta-adrenoceptor blocker diversity is represented in differences in beta-receptor selectivity of the blockade, the presence or absence of intrinsic sympathomimetic activity, the existence of dual alpha-beta blockade in some cases, differing lipophilicity, and a vascular vasodilatory action possessed by some beta blockers.
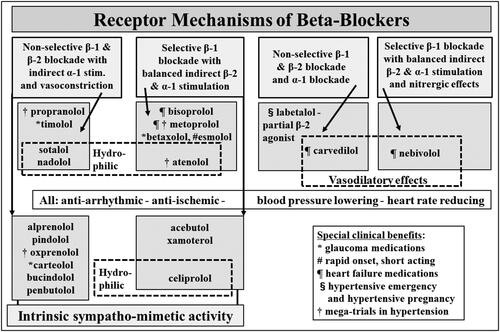
Table 1. Overview of beta-blockers and properties with the various compounds.
Table 2. Overview of the use of beta-blockers on clinical indications in the randomised clinical trials of patients with heart failure with preserved ejection fraction (HFpEF).
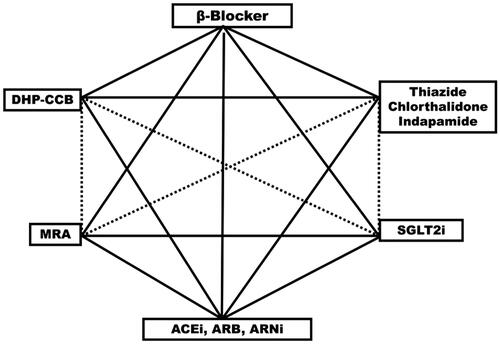
Figure 4. Hexagon shows suitable first-line drugs in the treatment of hypertension. Solid lines connect drug classes in combinations documented to prevent cardiovascular complications in hypertension or hospitalisation and death in randomised placebo controlled clinical trials in patients with heart failure with predominantly hypertensive aetiology. ACEi: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; ARNi: angiotensin receptor blocker neprilysin inhibitor; MRA: mineralocorticoid receptor antagonist; SGLT2i: sodium glucose cotransporter inhibitor; DH-CCB: dihydropyridin calcium channel blocker (calcium-antagonist)