Figures & data
Table 1. Characteristics of included studies.
Figure 2. Hazard ratios of overall long-term mortality between PCI and CABG in patients with chronic kidney disease. PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; SE: standard error; CI: confidence interval.
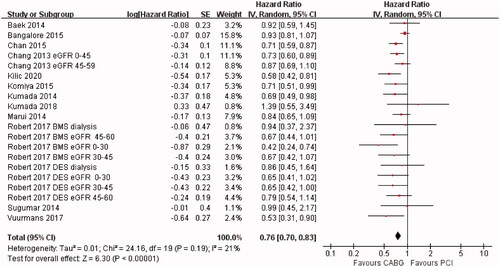
Figure 3. Hazard ratios of overall long-term mortality between PCI and CABG in patients on dialysis. PCI: percutaneous coronary intervention. CABG: coronary artery bypass surgery; SE: standard error; CI: confidence interval.
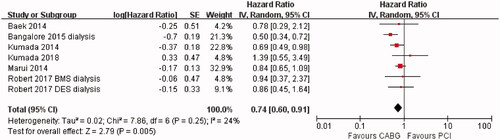
Figure 4. Hazard ratios of overall long-term mortality between CABG and PCI in patients with eGFR < 30 and eGFR > 30. PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; eGFR: estimated glomerular filtration rate; SE: standard error; CI: confidence interval.
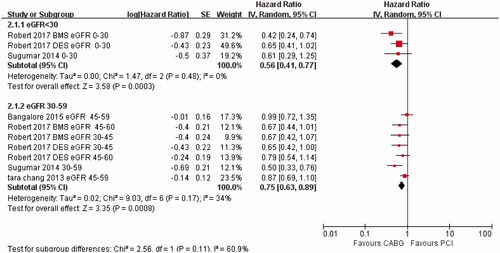
Figure 5. Hazard ratios for overall long-term mortality between CABG and PCI in patients with eGFR < 45 and eGFR > 45. PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; eGFR: estimated glomerular filtration rate; SE: standard error; CI: confidence interval.
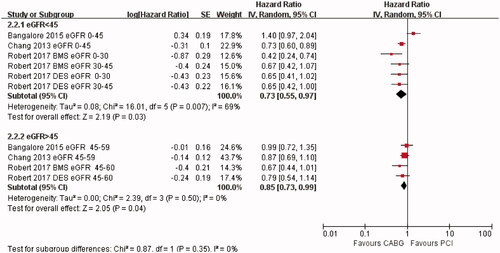
Figure 6. Comparison of secondary outcomes (myocardial infarction (MI), revascularization, and stroke) between CABG and PCI in patients with chronic kidney disease. PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; CI: confidence interval.
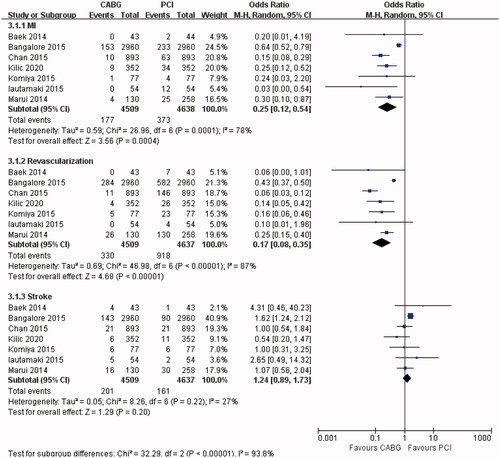
Figure 7. Secondary outcomes (myocardial infarction (MI), revascularization, and stroke) between CABG and PCI in patients on dialysis. PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; CI: confidence interval.
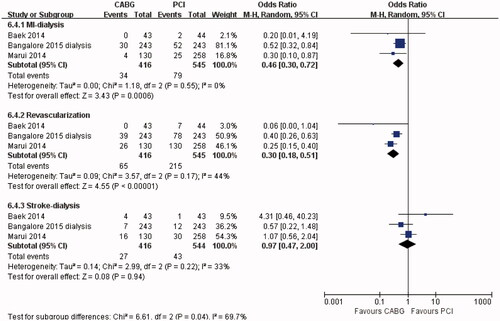
Table 2. Results of the main analysis.
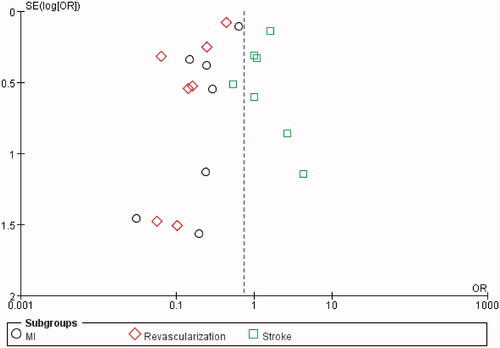
Figure 9. Funnel plot for odds ratios for myocardial infarction (MI), revascularization, and stroke.
Supplemental Material
Download PDF (390.4 KB)Data availability statement
All data and materials used in this research are freely available. References have been provided.