Figures & data
Table I. Comparison of general data of the two groups of patients.
Figure 1. Comparison of Maryland scale between two groups of patients before and after treatment. P < .05, the difference is statistically significant. Before treatment: control group 35.36 ± 5.02; L-PRF group 34.52 ± 5.29,t = 0.513,p = .600; After treatment: control group 88.84 ± 5.22; L-PRF group 94.80 ± 4.14,t=−4.499,p<.001.
Figure 2. Comparison of SF-36 quality of life scale between two groups of patients before and after treatment.Pf: physical functioning, RP: role- physical, BP: bodily pain, GH: general health, VT: validity, SF: social function, RE: role-emotional, MH: mental health. P < .05, the difference is statistically significant. There were statistically significant differences between the preoperative and postoperative comparisons of each item in the control group. The scores of each item in the L-PRF group after operation were significantly higher than those before operation. P-values are shown in the figure. *: Indicates that there is a statistically significant difference between the scores after treatment and the corresponding scores before treatment. There was no statistical significance in the comparison of SF-36 quality of life scale between the two groups during the same period.
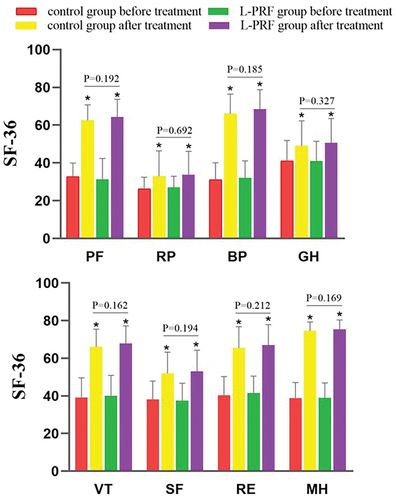
Table II. Treatment conditions and complication rates of the two groups of patients.
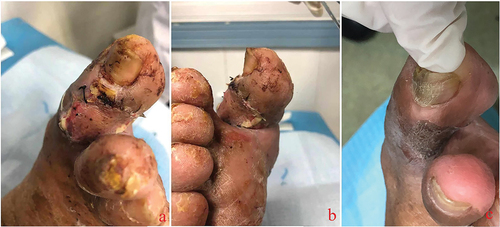
Figure 3. Most diabetic foot wounds start from lesions of the small blood vessels at the distal end of the affected limb. The destruction of the local blood supply impairs survival of the skin and soft tissue of the toe. At this time, the skin of the affected toe is often darkened (a), and mild paresthesia is often combined. Then, local skin necrosis occurs, subcutaneous tissue is exposed, ulcer wounds are formed (b), and the sensory function of the affected toe is impaired. Due to impaired sensory function, the pain is not severe despite the severe wound. The continuous necrosis of the surrounding tissue and the high probability of trauma make the wound develop further, and tendons and bones are gradually exposed (c, d). Local infection can occur at various stages after wound formation.

Figure 4. In the initial treatment of diabetic foot ulcer wounds, sufficient debridement was given to completely remove necrotic tissue. Tendons and bones were exposed after the debridement of most toe wounds (a the first day after debridement). The first day after debridement (b), we used L-PRF to cover the wound. The third day after debridement (c), we again performed wound dressing and covered the wound with L-PRF. The 5th day after debridement (d), after removing the wound dressing we can see that the wound surface was tidy, the wound area was slightly reduced, no necrosis and abnormal secretions were seen.

Figure 5. After successful reconstruction of the transplanted wound bed, anterior tibial free skins were used for skin grafting. The L-PRF group had a higher rate of skin graft survival, the well-surviving skin had no necrosis or infection, and the color of the skin was similar to that of normal tissue. (a, b). Well-recovered skin at an average of one-year postoperative follow-up showed good coverage of the ulcer wounds (c). The hyperplasia and skin graft area had good abrasion resistance.