Figures & data
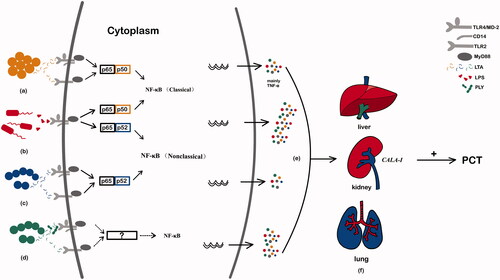
Table 1. Overview of common pathogens and their associations with procalcitonin.