Figures & data
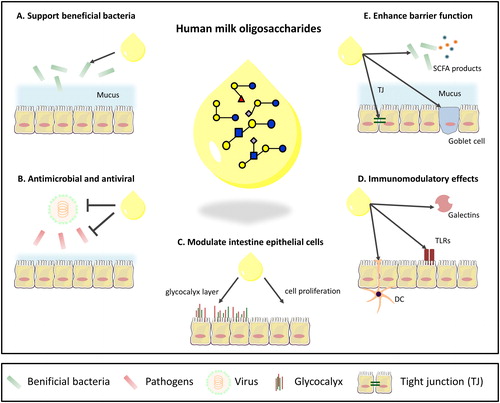
Figure 1. The intestinal immune barrier. (A) The small intestinal immune barrier. The mucus and the underlying closely connected epithelial cells form a barrier between the immune system and luminal content, which contains food and microbiota. Different cells contribute to the maintenance of barrier function and to balancing immune responses. These include intestinal epithelial cells, M cells, Paneth cells, stem cells and goblet cells. The immune components of the gut-associated lymphoid tissue are localized in Peyer’s patches, mesenteric lymph nodes, and lamina propria. (B) The large intestine. Colonocytes and goblet cells are the major cell types of the colonic crypt. Goblet cells produce mucus to form the outer and inner mucus layer which serves as protective barrier. The outer mucus layer harbors the commensal flora.
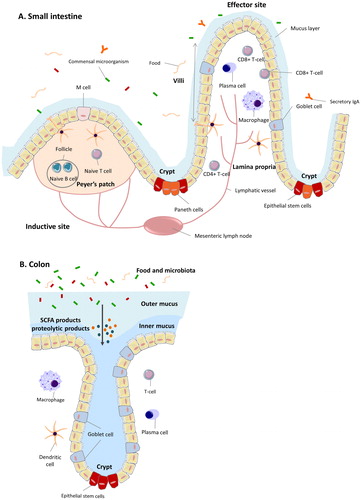
Figure 2. Structures of hMOs. (A) Building blocks and structural blueprint of hMOs. (B) Lactose can be elongated by addition of either lacto-N-biose (type I) or N-acetyllactosamine (type II) disaccharides. The addition of a β1-6 linkage produces branched structures (iso-hMO); the β1-3 linkage leads to linear structures (para-hMO). (C) Lactose is fucosylated or sialylated through different linkages to generate trisaccharides. (D) Galactosyl residues are linked to lactose through β1-3, β1-4- and β1-6 linkages to form galactosyllactoses. (E) Elongated type I or II chains can be fucosylated or sialylated in different linkages to form a variety of structural isomers.
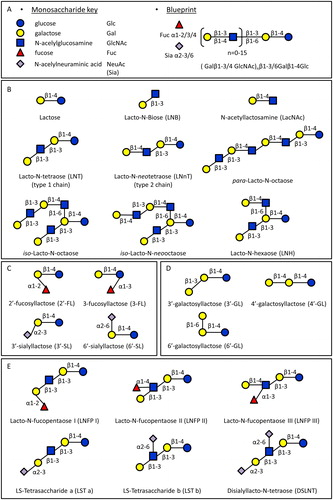
Figure 3. Overview of known functions of hMOs in the intestine. (A) Support the growth and colonization of beneficial bacteria. (B) Antimicrobial and antiviral effects by serving as decoy for pathogens and/or inhibit the growth of pathogens. (C) Exert a direct influence on intestinal epithelial cells by enhancing barrier function. (D) Immunomodulatory effects. (E) Effects on intestinal barrier function.