Figures & data
Figure 1. Gross observation of the stent-graft at the sacrifice of the animal: (A) encapsulated prosthetic aneurysm fitted with a stent-graft in situ before explantation; (B1, B2) encapsulated prosthetic aneurysm representative of the 25 specimens whose encapsulations was classified as excellent.
Figure 2. Different shapes of the stent-grafts (SG) after explantation and fixation in formaline; (A1, A2) representative device of 12 straight SGs; (B1, B2) representative device of 12 slightly SGs; (C1, C2) representative specimen of 4 bent SGs; (D1, D2) sole misaligned device.
Figure 3. IUVS illustrations of the lumen and cross-section of explanted stent graft; (A) thin internal capsule with some scattered mural thrombi in the area of anchoring Module A and Module B; (B) scattered mural thrombus resulting from alteration of the shape of the stent-graft.
Figure 4. Illustration in endoscopy of the luminal surface of the stent-grafts. (A) distal end of the transrenal stent constriction in a stent-graft; (B) constriction at the anchorage of Module B in Module A with variable levels of thrombotic anchorages in a stent-graft.
Figure 5. Gross observation after dissection of a stent-graft implanted for 3 months. The flow surface of the proximal and distal segments, i.e., contact with the host artery, are smooth and glistening. Proximally, the blood supply of the kidney does not suffer impairment as the bare stent is kept open vis-à-vis the ostia of the left kidney artery (double arrows). The luminal surface of the medium segment is immature as bare stent struts and polyester knit are exposed to the blood flow (triple arrows). The stent-graft holds a reorganized sac capsule while the blood thrombus in the aneurismal sac has fully solidified but its reorganization is limited to the area in contact with the polyester of the stent-graft (X). The prosthetic aneurysm is well encapsulated (XX). Distally, the internal capsule encompasses all the bare stent (arrow head) with some minor mural thrombi (double arrow heads) while the distal extremity of the stent causes some overdistension of the aorta (triple arrow heads).
Figure 6. Scanning electron microphotography of the proximal section of the Module A in a stent-graft explanted six months after implantation. The struts of the stent are embedded in a very thin fragile capsule whose splitting is probably due to specimen processing (arrow). The flow surface of the artery beneath the stent is smooth and glistening with an intimate contact with the stent (A:×27). The entrance of the left kidney is kept open preventing impairment in the blood supply (B:×27).
Figure 7. Scanning electron microphotography of the proximal segment of the Module A. This stent-graft was implanted for 6 months. In the areas of contact between the stent and the host artery the struts of the stent are well incorporated (double arrows) and the flow surface is well healed with the presence of a vasa-vasorum (arrows) (A:×22) whose ostia is well defined (arrow heads) and luminal surface covered with a continuous layer of endothelial cells (B:×600).
Figure 8. Scanning electron microphotography of the luminal surface of the most proximal segment of the Module B implanted for 12 days. It shows the bare stent (single arrows) and with some minor blood debris (double arrows) above the polyester impregnated with a thrombotic matrix that makes the prosthetic wall impervious to blood percolating (A*;B**) (A:×23) (B:×23).
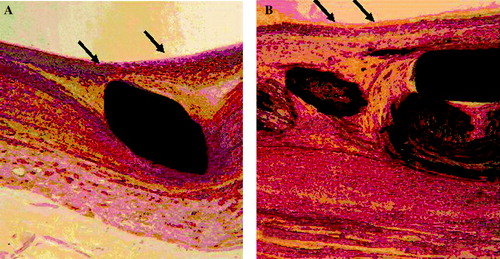
Figure 9. Histology of the section at the level the left renal artery in a stent-graft implanted for six months. The internal capsule is well developed with endothelial-like cells on the flow surface (arrows). Such a capsule is made of collagen incorporating numerous cells (fibroblasts and smooth muscle cells) without any necrotic tissue: stent only (A:×200) and stent and polyester (B:×200).