Figures & data
Figure 1. The primary pathogenesis of psoriasis. Genetic, environmental, and immunological factors induce active oxidative stress (OS) responses, leading to increased reactive oxygen species (ROS), malodialdehyde, nitric oxide, superoxide, inducible nitric oxide synthase, and decreased catalase, superoxide dismutase, and glutathione peroxidase in psoriatic lesions and in serum. Abnormal OS follows excessive ROS production, active dendritic cells, mast cells, macrophages and neutrophils, and activated nuclear factor kappa B, mitogen activated protein kinase, and Janus kinase-signal transducers and activators of transcription signaling pathways. Under these conditions, cells secrete proinflammatory cytokines, including IL-12, 17, 19, 22, 23, tumor necrosis factor alpha (TNF-α), interferon-gamma (IFN-γ), and transforming growth factor beta. Released cytokines promote the expression of vascular endothelial growth factor and encourage Th1/Th17 cell activation and decreased Treg cell activity. Increased numbers of Th1 and Th17 cells secrete IFN-γ, TNF-α, IL-17, IL-21, IL-22, IL-23, and IL-26, and subsequent STAT3 signaling leads to increased keratinocyte numbers, thus contributing to psoriasis. OS, oxidative stress; ROS, reactive oxygen species; NO, nitric oxide; MDA, malondialdehyde; , superoxide radical; SOD, superoxide dismutase; GSH-PX, glutathione peroxidase; CAT, catalase; DCs, dendritic cells; IL, interleukin; TNF-α, tumor necrosis factor alpha; TGF-β, transforming growth factor beta; IFN-γ, interferon-gamma; STAT3, signal transducers and activators of transcription; Th, T helper; Treg cells, regulatory T cells; VEGF, vascular endothelial growth factor; KCs, keratinocytes.
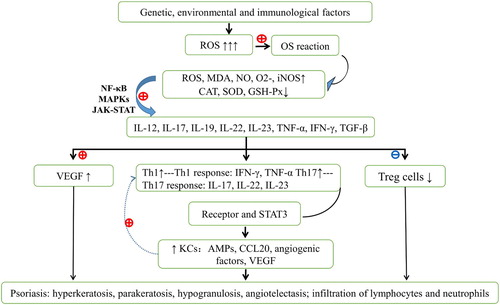
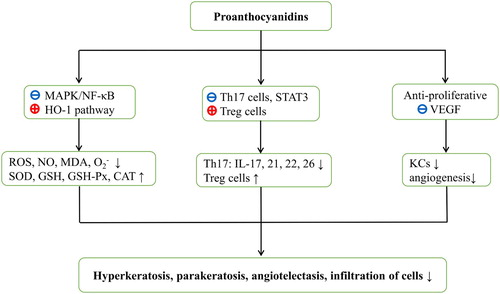
Figure 2. Hypothesized mechanisms of action of proanthocyanidins against psoriasis. Proanthocyanidins block MAPK/NF-κB signaling pathways and activate HO-1 expression. Oxidative stress parameters such as reactive oxygen species and malondialdehyde are then decreased with increasing antioxidant levels. Proanthocyanidins also reduce Th17 cell numbers and moderate the release of STAT3-dependent cytokines. Moreover, increased Treg cell numbers in the presence of proanthocyanidins may facilitate immunological tolerance. Furthermore, proanthocyanidins are anti-proliferative and may prevent VEGF expression. Ultimately, all these aspects are likely to contribute to the control of psoriasis. ROS, reactive oxygen species; NO, nitric oxide; MDA, malondialdehyde; , superoxide radical; SOD, superoxide dismutase; GSH-PX, glutathione peroxidase; GSH, glutathione; CAT, catalase; STAT3, signal transducers and activators of transcription; Th, T helper; Treg cells, regulatory T cells; IL, interleukin; VEGF, vascular endothelial growth factor; KCs, keratinocytes.