Figures & data
Figure 2. Patient selection flowchart. ICD-9, International Classification of Diseases, 9th Revision; LAI, long-acting injectable antipsychotic; OM, once monthly; TM, twice monthly.
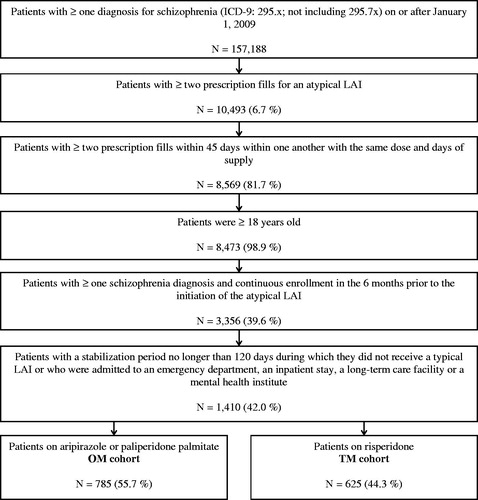
Table 1. Patient characteristics during the baseline period.
Figure 3. Comparison of persistence to index medication during the first 2 years following the index year. CI, confidence interval; HR, hazard ratio; OM, once monthly; TM, twice monthly. *Significant at the 5% level. aAdjusted models controlled for demographics (age, sex, race/ethnicity); region of residence (state, urban/rural area); year of the index date, number of unique mental health diagnoses recorded during the baseline period; number of unique antipsychotic agents received during the baseline period; comorbidities at baseline (diabetes, cardiovascular diseases, substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, depressive disorders, Quan-Charlson Comorbidity Index); number of outpatient, 1-day mental-health institute, inpatient, and emergency room visits during the baseline period; total costs at baseline; Medicare eligibility; and risperidone dose equivalence on the index date. bOM patients vs TM patients: An HR <1 means that TM patients have a higher risk of discontinuing their index drug than OM patients.
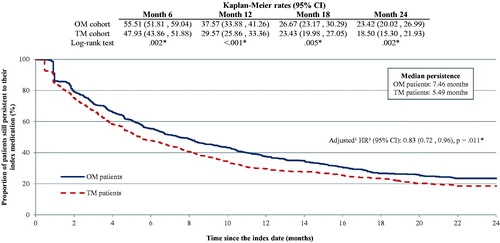
Figure 4. Inpatient utilization during the first 12 months following the index date. *Significant at the 5% level. IRR, incidence rate ratio; OM, once monthly; SD, standard deviation; TM, twice monthly. aAdjusted models controlled for demographics (age, sex, race/ethnicity); region of residence (state, urban/rural area); year of the index date; number of unique mental health diagnoses recorded during the baseline period; number of unique antipsychotic agents received during the baseline period; comorbidities at baseline (diabetes, cardiovascular diseases, substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, depressive disorders, Quan-Charlson Comorbidity Index); number of outpatient, 1-day mental-health institute, inpatient, and emergency room visits during the baseline period; total costs at baseline; Medicare eligibility; and risperidone dose equivalence on the index date. bIRRs, 95% CIs, and p-values were estimated using a generalized linear model (GLM) with a negative binomial distribution.
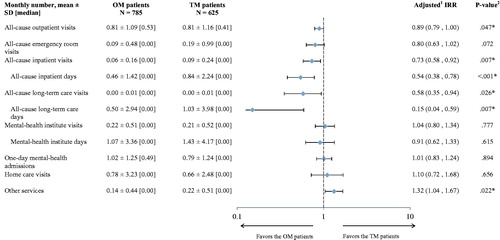
Table 2. Healthcare costs during the first 12 months following the index date.