Figures & data
Table 1. Individual supply use from the Reveal LINQ ICM supply kit.
Figure 1. Time intervals according to procedure location. Box plots represent the duration of different procedure time intervals according to procedure location in-office or in-hospital.
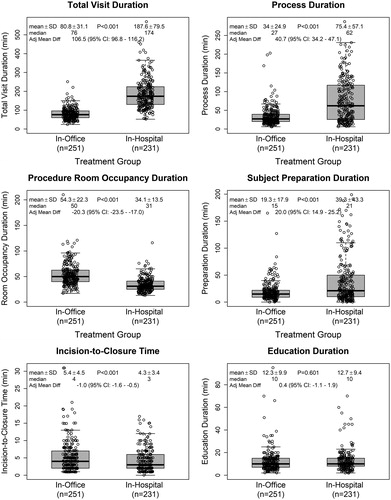
Figure 2. Definitions of time intervals recorded during the study. Total visit duration (time from patient check-in to discharge, including all waiting periods); process duration (time from the start of the patient preparation to incision closure, including the wait time between patient preparation and the start of device insertion); procedure room occupancy duration (time from when patient entered the procedure room to when they exited; variable whether education was delivered in the same room as the procedure or in a different location); patient preparation duration (time required for clinical assessment, changing clothes and surgical site preparation); incision-to-closure time (procedure duration); and patient education (time required to educate patients on the use of their ICM device and care of their insertion wound).
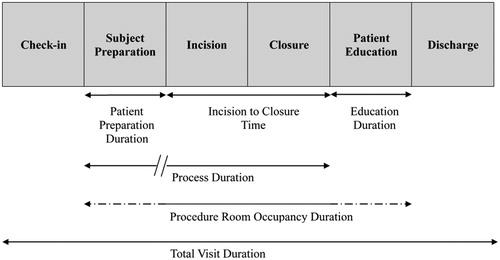
Figure 3. Relationship between number of ICM insertion procedures at each study center and total visit duration (left panel) and process duration (right panel). Point size is proportional to the number of ICM insertion procedures performed. Solid lines indicate predicted average duration and dashed lines display the 95% confidence intervals for the predicted average.
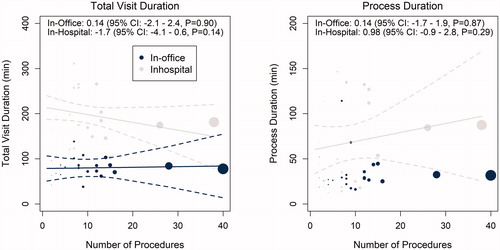
Table 2. Pre-insertion resource utilization.
Figure 4. Staff involvement at each phase of the procedure: pre-insertion (left panel), insertion (center), and post-insertion (right). *p-value < 0.001 calculated by repeated measures logistic regression model using generalized estimating equations to account for multiple patients at each study site. †Nurse practitioners participated in nine insertion procedures at three study sites. ‡Physician assistants participated in nine insertion procedures at one study site. §Nurse practitioners participated in post-procedure education activities following five procedures at one study site. ∥Physician assistants participated in post-procedure education activities following 10 procedures at three sites.
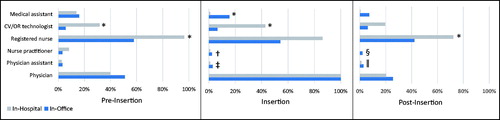
Table 3. Staffing costs.
Table 4. Cost of supply use from the Reveal LINQ ICM supply kit.
