Figures & data
Table 1. Patient characteristics.
Figure 1. IRR of HE-related and all-cause IP admissions and days during rifaximin versus lactulose episodes in the Marketscan database. Abbreviations. CCI, Charlson comorbidity index; CI, confidence interval; DRG, diagnosis-related group; HE, hepatic encephalopathy; IP, inpatient; IRR, incidence rate ratio; PDC, proportion of days covered; SD, standard deviation.
Notes: aHE-related hospitalizations were defined as hospitalizations with HE as primary diagnosis, as well as DRG 441, 442, or 443 (liver-related diseases).
bFor the secondary scenario, HE-related hospitalizations were defined as hospitalizations with HE as primary or secondary diagnosis.
cModels were adjusted for age, gender, region, health plan, baseline procedures (paracentesis, endoscopy, transvenous intrahepatic portosystemic shunt, and dialysis) and Charlson comorbidity index.
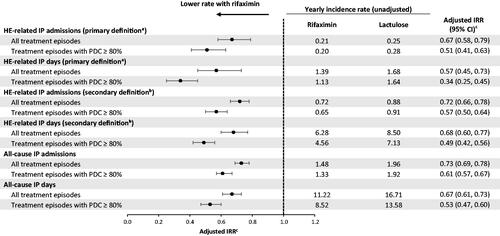
Figure 2. IRR of HE-related and all-cause IP admissions and days during rifaximin versus lactulose episodes in the Optum database. Abbreviations. CCI, Charlson comorbidity index; CI, confidence interval; DRG, diagnosis-related group; HE, hepatic encephalopathy; IP, inpatient; IRR, incidence rate ratio; PDC, proportion of days covered; SD, standard deviation.
Notes: aHE-related hospitalizations were defined as hospitalizations with HE as primary diagnosis, as well as DRG 441, 442, or 443 (liver-related diseases).
bFor the secondary scenario, HE-related hospitalizations were defined as hospitalizations with HE as primary or secondary diagnosis.
cModels were adjusted for age, gender, region, health plan, baseline procedures (paracentesis, endoscopy, transvenous intrahepatic portosystemic shunt, and dialysis) and Charlson comorbidity index.
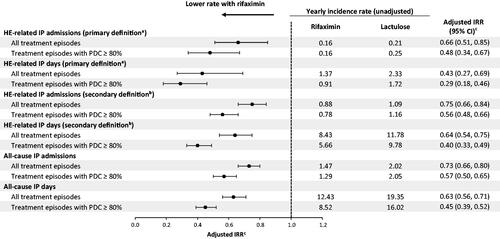
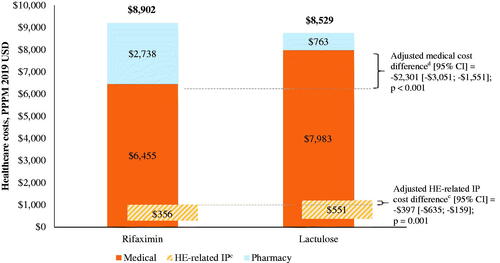
Figure 3. Healthcare costs among patients during rifaximin versus lactulose episodes in the Marketscan databasea,b. Abbreviations. CI, confidence interval; DRG, diagnosis-related group; HE, hepatic encephalopathy; IP, inpatient; PPPM, per-patient-per-month; USD, United States dollar.
Notes: aMean costs presented are unadjusted, while cost differences were weighted using episode duration and adjusted for age, gender, region, health plan, Charlson comorbidity index during baseline, and procedures during baseline (i.e. paracentesis, dialysis, endoscopy, transvenous intrahepatic portosystemic shunt).
bThe mean medical and pharmacy costs were estimated from separate unadjusted models and therefore do not sum to the total healthcare costs.
cHE-related IP costs were defined as those from hospitalizations with HE as primary diagnosis, as well as DRG 441, 442, or 443 (liver-related diseases). For the secondary scenario (hospitalizations with HE as primary or secondary diagnosis), unadjusted HE-related IP costs were $2,219 in the rifaximin cohort and $3,108 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$1,235 (–$1,655; –$814); p < .001. Unadjusted all-cause IP costs were $3,990 in the rifaximin cohort and $5,679 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$2,054 (–$2,613; –$1,495); p < .001.
dUnadjusted pharmacy costs were $2,760 in the rifaximin cohort and $921 in the lactulose cohort, with an adjusted cost difference (95% CI) of $1,878 ($1,742; $2,014); p < .001. Unadjusted outpatient costs were $2,283 in the rifaximin cohort and $2,255 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$180 (–$343; –$17); p = .030.
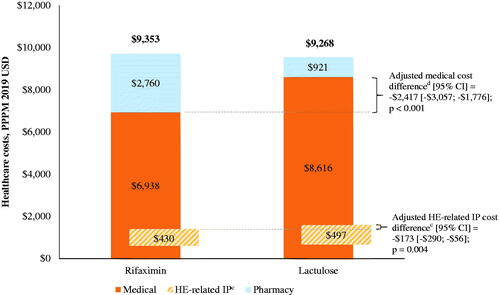
Figure 4. Healthcare costs among patients during rifaximin versus lactulose episodes in the Optum databasea,b. Abbreviations. CI, confidence interval; HE, hepatic encephalopathy; IP, inpatient; PPPM, per-patient-per-month; USD, United States dollar.
Notes: aMean costs presented are unadjusted, while cost differences were weighted using episode duration and adjusted for age, gender, region, health plan, Charlson comorbidity index during baseline, and procedures during baseline (i.e. paracentesis, dialysis, endoscopy, transvenous intrahepatic portosystemic shunt).
bThe mean medical and pharmacy costs were estimated from separate unadjusted models and therefore do not sum to the total healthcare costs.
cHE-related IP costs were defined as those from hospitalizations with HE as primary diagnosis, as well as DRG 441, 442, or 443 (liver-related diseases). For the secondary scenario (hospitalizations with HE as primary or secondary diagnosis), unadjusted HE-related IP costs were $2,372 in the rifaximin cohort and $3,175 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$1,693 (–$2,312; –$1,075); p < .001. Unadjusted all-cause IP costs were $3,497 in the rifaximin cohort and $4,901 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$2,113 (–$2,765; –$1,462); p < .001.
dUnadjusted pharmacy costs were $2,738 in the rifaximin cohort and $763 in the lactulose cohort, with an adjusted cost difference (95% CI) of $1,978 ($1,802; $2,155); p < .001. Unadjusted outpatient costs were $2,295 in the rifaximin cohort and $2,307 in the lactulose cohort, with an adjusted cost difference (95% CI) of –$35 (–$280; $211); p = .782.