Figures & data
Figure 1. Sample attrition for VNS and RNS/DBS cohorts. All percentages above are calculated using the population from the prior category. As neurostimulation may be used for several indications (e.g., epilepsy, Parkinson's disease, essential tremor), we required the presence of a diagnosis of epilepsy on the date of procedure to maximize the likelihood that the patient received implantation for treatment of epilepsy; to provide further confirmation of chronic epilepsy (a prerequisite for consideration of neurostimulation), the longer 1-year period was applied to assess ASM use. The cohorts therefore represented patients with evidence of: (1) chronic epilepsy; (2) ASM use; and (3) use of neurostimulation for epilepsy.
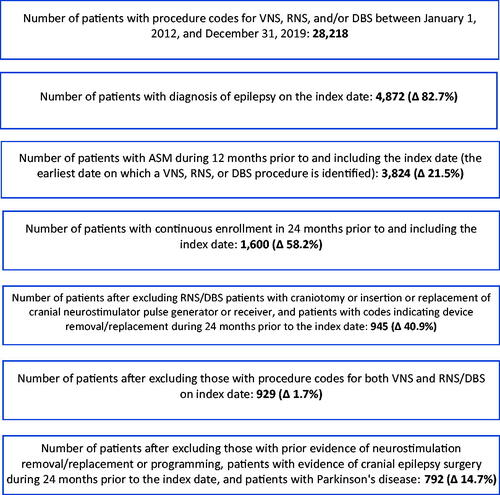
Table 1. Demographic and clinical characteristics on index date, by match status and cohort.
Table 2. Healthcare resource following neurostimulation.
Table 3. Healthcare costs following neurostimulation, by time period of interest.
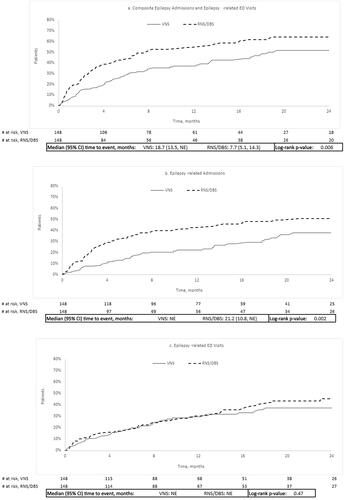
Figure 2. Kaplan–Meier time to event analyses. (a) Composite of epilepsy-related admissions and epilepsy-related ED visits, (b) epilepsy-related admissions, and (c) epilepsy-related ED visits. Abbreviations. CI, confidence interval; DBS, deep brain stimulation; ED, emergency department; NE, not estimable; RNS, responsive neural stimulation; VNS, vagus neural stimulation.
Appendix 1. Patient identification using procedure and diagnostic codes.
Appendix 2. ASM medications.
