Figures & data
Figure 1. Patient 1 at 6 years of age. There is significant disruption of the inner retina with marked thickening and loss of normal foveal contour. Central subfield thickness (ILM-RPE) is 529 microns.
Figure 2. (a) Patient 1 at 7 years of age. SD-OCT reveals grossly abnormal contour and thickening of the outer retina with no apparent foveal depression. Central subfield thickness (ILM-RPE) is 500 microns. SD-OCT one year earlier also showed thickening, loss of contour, and gross contour changes (). Fundus photograph shows yellowish hue within the macula with loss of foveal reflex, radial retinal striations, and pinpoint white deposits nasal to the fovea. The ffERG shows borderline low LA 3.0 and below-normal LA 28 Hz amplitude cone-mediated ERGs. Rod-mediated were markedly depressed to the DA 0.01 flash strength and in mixed rod-cone DA 3.0 and DA 10.0 A- and B-waves. (For all patients, with the exception of the DA 10.0 condition, two successive ERG recordings from the right eye are shown. The rectangles on each recording denote the expected amplitude and implicit time limits for the LA and DA ERGs provided by the manufacturer). (b) Patient 2, the 5-year-old affected sibling. SD-OCT reveals abnormal foveal contour with loss of foveal depression as well as areas of thickening and elevation. Central subfield thickness (ILM-RPE) is 411 microns. Fundus photograph shows blunted foveal reflex, macular striations, and small, pinpoint, hypopigmented macular deposits. The ffERG shows a pattern of loss similar to her 7-year-old sibling (a) with a reduction in cone-mediated LA ERG, most notable in the LA 28 Hz condition. Rod-mediated B-wave ERGs to the DA 0.01 flash strength were relatively less affected in Patient 2, but the amplitude of the A-waves in the mixed DA 3.0 and 10.0 conditions were clearly reduced compared with normal range and the older sibling, Patient 3. (c) Patient 3, the 12-year-old unaffected sibling. SD-OCT reveals a normal, healthy retina. Central subfield thickness (ILM-RPE) is 257 microns. Fundus photograph shows normal macular findings and normal vessel findings. The ffERG shows LA and DA A- and B-waves within expected limits.
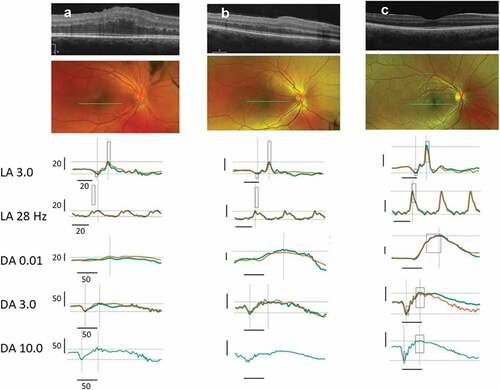
Figure 3. Patient 1: Yellowish hue within the macula with loss of fovea reflex; radial retinal striations OU; pinpoint white deposits noted nasal to the fovea OD. Patient 2: Blunted foveal reflex, macular striations, small pinpoint, hypopigmented macular deposits OU. The deposits are hypo-AF on AF OU. Normal appearing optic nerve and retinal vessels OU. Patient 3: Findings include normal observations. Disc findings include normal observations. Macula findings include normal observations. Periphery findings include normal observations. Vessel findings include normal observations.