Figures & data
Table 1. Baseline characteristics.
Table 2. Prevalence of ECG findings in patients with different ST-elevation etiology.
Table 3. Reciprocal ST-segment changes in patients with anterior or inferior ST elevation.
Table 4. ECG findings to be used to detect patients with STEMI: Sensitivity, specificity and likelihood ratio for an ischemic etiology.
Table 5. ECG findings to be used to detect non-ischemic patients: Sensitivity, specificity and likelihood ratio for a non-ischemic etiology.
Table 6. Univariate and multivariable predictors of ischemic STE.
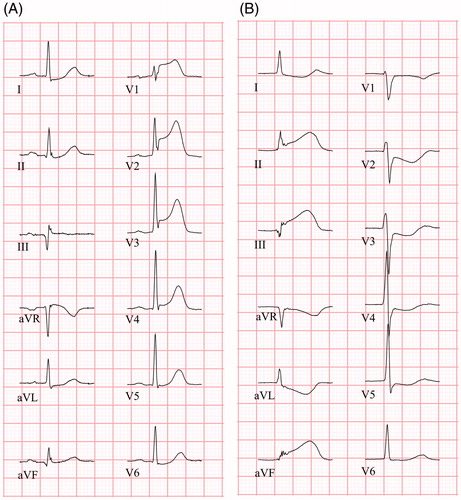
Figure 1. ECGs (25 mm/s) from four patients with different ST elevation etiologies. (A) Patient with STEMI. ECG shows PR depression ≥0.05 mV in the limb leads, but not in the chest leads, and slight ST elevation in aVR. (B–D) Non-ischemic patients with ST elevation (B: perimyocarditis; C: takotsubo cardiomyopathy; D: ERS). Both (B) and (C) show PR depression in both limb leads and chest leads, in (D) minor PR depression is present in the limb leads, and PR depression ≥0.05 mV in lateral chest leads. All non-ischemic patients show some degree of ST depression in aVR.
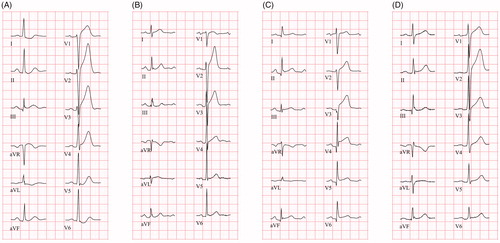
Figure 2. ECGs (25 mm/s) from two STEMI patients. (A) ECG shows concave ST elevation in V1 – V4 and ST depression in aVL, I and II. ST elevation is present in aVR. PR depression is absent in both limb leads and chest leads. Terminal QRS distortion is present in leads V2 and V3 (absent S and J wave in leads with ST elevation (Rs configuration)). (B) ECG shows concave ST elevation in inferior leads (II, aVF, III) with reciprocal ST depression in leads aVL and I, as well as precordial leads. PR depression is absent in both limb leads and chest leads. Terminal QRS distortion is present in aVF and III (ST elevation ≥50% of R-wave amplitude).