Figures & data
Figure 1. Examples of personalized care and integrated services of an innovative outcome-based care and procurement model. The goal of the Innovative Outcome-based Care and Procurement Model is to efficiently provide clotting factors to people with hemophilia. Here we list potential supportive tools for physicians and patients grouped according to trough levels and bleeding frequency to reduce or eliminate bleeds.
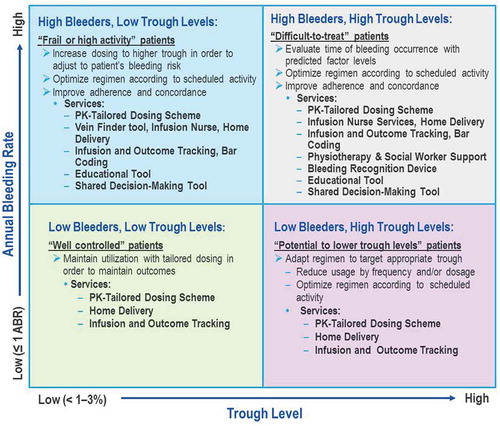
Figure 2. Innovative outcome based care and procurement: the ins and outs. This model is facilitated through the integration of real-world data collection, tailored care and patient empowerment into personalized care. Outcome-based care thereby produces an opportunity for innovative procurement and improved outcomes, which result in increased value for money.
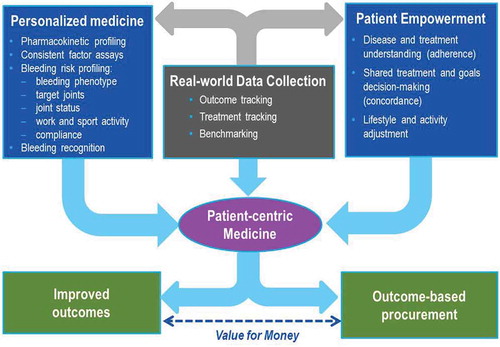
Figure 3. Self management and adherence: crucial for optimized outcomes: non-adherence in chronic disease is estimated to cost $100 billion per year in the US, or 4.5% of total healthcare spending,3 due to avoidable hospitalization costs alone. Total cost of non-adherence to the system is the probably much greater. Sources: aLorig and Holman, 2003; bSchrijvers, et al. 2013; cZappa et al., 2012; dClinical trial: ‘Nurse facilitated adherence therapy for haemophilia’, 2014. 3New England Healthcare Institute. ‘Thinking Outside the Pillbox: A Systemwide Approach to Improving Patient Medication Adherence for Chronic Disease’. A NEHI Research Brief. August 2009.
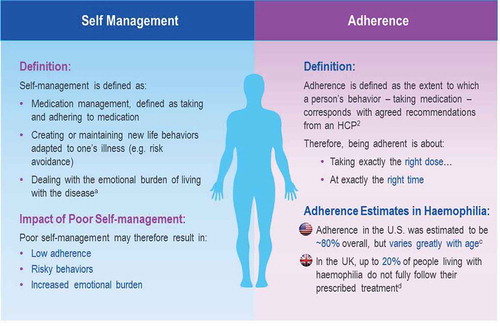
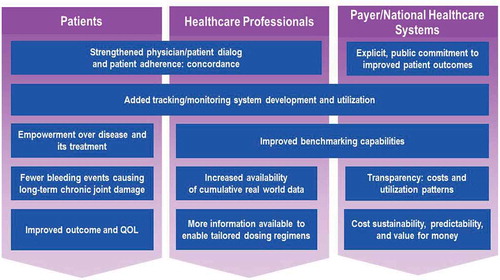
Figure 4. Innovative outcome-based care and procurement model stakeholder benefits. By aligning the goals of all stakeholders involved with hemophilia treatment to improve outcomes, the innovative outcome-based care and procurement model should provide significant benefits. The foundation for these benefits would begin with increased motivation to partake in increased concordance between patient and physician, built upon by improved tracking and monitoring systems to provide individual treatment plan comparability as well as increased cumulative benchmarking data. In addition, by supporting such a procurement policy, the payer demonstrates his/her commitment to the improvement of patient outcomes.