Figures & data
Figure 1. Menstrual cycle and migraine frequency. In this figure, serum levels of hormones and their effect on the endometrium over the course of the menstrual cycle are depicted, as well as the concurrence of fluctuations in the incidence of migraine attacks in women with menstrual migraine. Lasting around 28 days, the cycle starts with the release of FSH, stimulating the growth of ovarian follicles. The maturation of these follicles leads to an increasing production of estradiol, which triggers a surge in LH and causes ovulation. After ovulation, the ruptured follicle transforms into the corpus luteum which produces progesterone and prepares the endometrium for possible fertilization. If fertilization does not occur, the corpus luteum breaks down progesterone and estradiol levels drop, which triggers menstruation and the start of a new menstrual cycle [Citation23]. The decline of estradiol, also referred to as estradiol-withdrawal, is also thought to precipitate a migraine attack without aura in women with menstrual migraine [Citation24]. The figure is based on the data from Martin et al. [Citation25] and MacGregor et al. [Citation26] and was created using BioRender.
![Figure 1. Menstrual cycle and migraine frequency. In this figure, serum levels of hormones and their effect on the endometrium over the course of the menstrual cycle are depicted, as well as the concurrence of fluctuations in the incidence of migraine attacks in women with menstrual migraine. Lasting around 28 days, the cycle starts with the release of FSH, stimulating the growth of ovarian follicles. The maturation of these follicles leads to an increasing production of estradiol, which triggers a surge in LH and causes ovulation. After ovulation, the ruptured follicle transforms into the corpus luteum which produces progesterone and prepares the endometrium for possible fertilization. If fertilization does not occur, the corpus luteum breaks down progesterone and estradiol levels drop, which triggers menstruation and the start of a new menstrual cycle [Citation23]. The decline of estradiol, also referred to as estradiol-withdrawal, is also thought to precipitate a migraine attack without aura in women with menstrual migraine [Citation24]. The figure is based on the data from Martin et al. [Citation25] and MacGregor et al. [Citation26] and was created using BioRender.](/cms/asset/c5be3984-393f-4c91-bd7f-7681f186cf9b/iern_a_2296610_f0001_oc.jpg)
Figure 2. Hormonal treatment of migraine, their advantages and disadvantages. this figure provides an overview of existing hormonal therapies, their benefits, risks and potential challenges. Figure was created using BioRender.
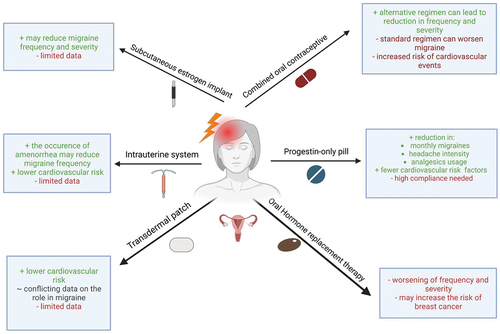
Table 1. Summary of the main original studies investigating the effect of hormonal treatments. Papers focusing on adverse events or case series are not included in this summary.
