Figures & data
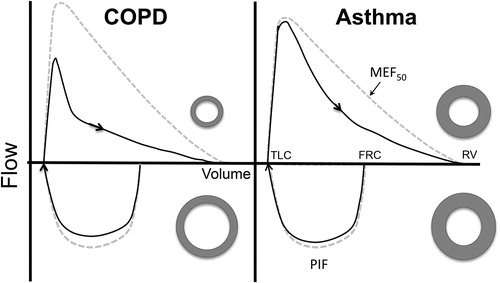
Figure 1. Flow-volume relationships for a theoretical patient with COPD (left hand panel) and for a patient with asthma (right hand panel) preformed using the technique for maximal inspiration described by Okazawa at all (4). Following a period of quiet breathing the patient takes a maximum inspiration from functional residual capacity (FRC) to total lung capacity TLC with a maximum expiration to residual volume (RV). From the expiratory limb the forced expiratory volume in one second (FEV1), forced vital capacity (FVC) are determined and maximum expiratory flow rate at 50% vital capacity (MEF50) is measured. In addition, maximum inspiratory flow (PIF) is measured from the inspiratory limb. For the patient with asthma, expiratory flow is diminished likely due to thickening of the airways with minimum compression during expiration and minimal tethering during inspiration. On the other hand, for the patient with COPD expiration is diminished in part due to compression of airways due to lost of parenchymal tethering; that is, the airways are functionally more dispensable. On inspiration the same airway is pulled open as illustrated by the adjacent donut shapes. As result the FEV1/FVC is reduced in both cases but more so the case of the patient was COPD. PIF/ MEF50 is increased in both cases; the more so in the case of patients with COPD, because of the relative preservation of inspiratory flow. As a result, using both indices would be predicted to better discrimination between the two forms of airways disease.