Figures & data
Table 1. Anthropometric characteristics and lung function parameters in healthy control subjects and all patients with COPD and in COPD patients divided according to the presence or absence of pulmonary hyperinflation at rest.
Figure 1. Individual values of mean latency (panel a) and mean amplitude (panel b) of cMAP in the stable COPD patients and matched control subjects enrolled in the study and subgroups of COPD patients divided according to the presence (IC < 80% pred.) or absence (IC ≥ 80% pred.) of pulmonary hyperinflation at rest. IC = Inspiratory Capacity.
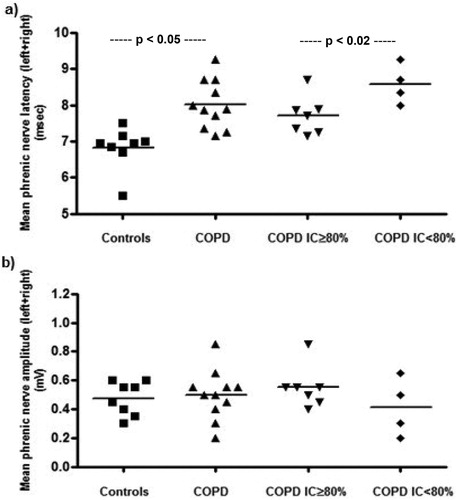
Figure 2. Correlation between values of mean latency of cMAP and resting IC (as % pred.) in stable COPD patients, suggesting an association between the prolonged velocity of conduction of phrenic nerves and degree of chronic pulmonary hyperinflation.
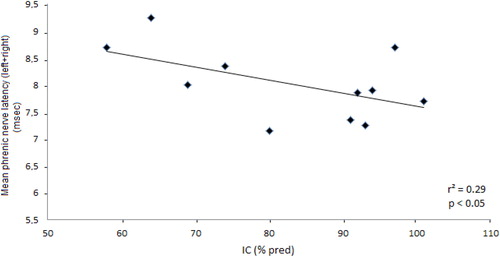
Table 2. Phrenic nerve conduction parameters in control subjects and all COPD patients, and in COPD patients divided according to the presence or absence of pulmonary hyperinflation at rest.
Figure 3. Individual values of amplitude and latency of cMAP during exacerbation (E) and at discharge (D) from the Hospital in a group of COPD patients hospitalized because of COPD exacerbation.
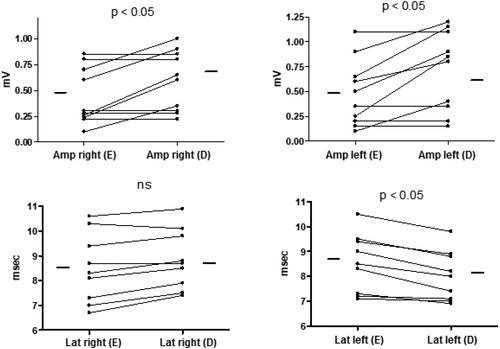
Table 3. Anthropometric characteristics, lung function parameters, and arterial blood gas values in a group of patients with COPD during exacerbation and at discharge.
Table 4. Phrenic nerve conduction parameters in a group of COPD patients during exacerbation and at discharge.
