Figures & data
Figure 1. Cumulative number of articles published from 1985 to 2020 related to OS, OSA, and COPD. To identify the number of published articles on OS, OSA, and COPD, searches were performed in MEDLINE using the search terms “chronic obstructive pulmonary disease” AND “obstructive sleep apnea,” “obstructive sleep apnea,” and “chronic obstructive pulmonary disease,” respectively. The numbers of published articles on OS, OSA, and COPD were 7, 119, and 390, respectively in 1985; the cumulative numbers of articles on OS, OSA, and COPD from 1985 to December 2020 were 1514, 41 236, and 79 430, respectively. OS: Overlap syndrome, OSA: Obstructive sleep apnea, COPD: Chronic obstructive pulmonary disease.
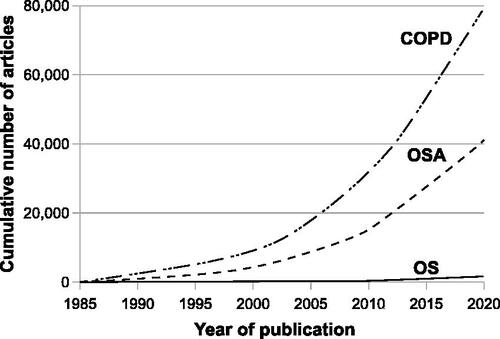
Figure 2. Diaphragm electromyogram (EMG) di% (left panel), ventilation (middle panel), and the VT/EMGdi (right panel) in patients with COPD alone, OS, normal subjects, and patients with OSA. EMGdi% (percentage of maximal diaphragm electromyogram) was used to assess neural respiratory drive. Upper airway resistance was inferred by the ratio of the tidal volume (VT) to EMGdi (VT/EMGdi). Ventilation decreases from wakefulness to sleep in all four groups, but the reduction is statistically significant only in patients with COPD, OS, and OSA. EMGdi decreases in patients with COPD alone but increases in patients with OSA from wakefulness to non-rapid eye movement sleep, whereas it remains the same in normal subjects and patients with OS. VT/EMGdi decreases from wakefulness to sleep in patients with OS and OSA but it changes little in normal subjects and patients with COPD alone. The decrease in ventilation is associated with a reduction of EMGdi in patients with COPD alone, whereas the reduction in ventilation is associated with decreased VT/EMGdi in patients with both OS and OSA. OSA: Obstructive sleep apnea, COPD: Chronic obstructive pulmonary disease, OS: Overlap syndrome. Adapted from [Citation31] (an open access article distributed in accordance with the Creative Commons Attribution Non Commercial [CC BY-NC 4.0] license).
![Figure 2. Diaphragm electromyogram (EMG) di% (left panel), ventilation (middle panel), and the VT/EMGdi (right panel) in patients with COPD alone, OS, normal subjects, and patients with OSA. EMGdi% (percentage of maximal diaphragm electromyogram) was used to assess neural respiratory drive. Upper airway resistance was inferred by the ratio of the tidal volume (VT) to EMGdi (VT/EMGdi). Ventilation decreases from wakefulness to sleep in all four groups, but the reduction is statistically significant only in patients with COPD, OS, and OSA. EMGdi decreases in patients with COPD alone but increases in patients with OSA from wakefulness to non-rapid eye movement sleep, whereas it remains the same in normal subjects and patients with OS. VT/EMGdi decreases from wakefulness to sleep in patients with OS and OSA but it changes little in normal subjects and patients with COPD alone. The decrease in ventilation is associated with a reduction of EMGdi in patients with COPD alone, whereas the reduction in ventilation is associated with decreased VT/EMGdi in patients with both OS and OSA. OSA: Obstructive sleep apnea, COPD: Chronic obstructive pulmonary disease, OS: Overlap syndrome. Adapted from [Citation31] (an open access article distributed in accordance with the Creative Commons Attribution Non Commercial [CC BY-NC 4.0] license).](/cms/asset/76f87762-5927-44cb-969a-2952c86d85c2/icop_a_1950663_f0002_b.jpg)
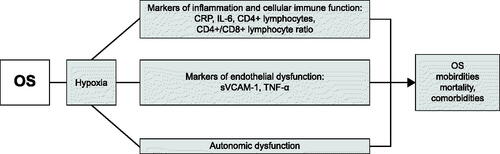
Figure 3. Markers of inflammation, endothelial dysfunction, and cellular immune function studied in OS patients. Whether these dysfunctions contribute to morbidity, mortality, and comorbidities associated with OS remain to be demonstrated. We did not speculate potential underlying mechanisms that have not been specifically elucidated in OS patients. OS: Overlap syndrome, CRP: C-reactive protein, IL-6: Interleukin-6, sVCAM-1: soluble vascular cell adhesion molecule-1, TNF-α: Tumor necrosis factor-α.