Figures & data
Table 1. Gamma camera radionuclides.
Table 2. positron emission tomography radionuclides.
Figure 1. 99mTc-pertechnetate scan presentation of Graves’ disease (a), autonomously functioning thyroid nodules (b) and destructive thyroiditis (c).
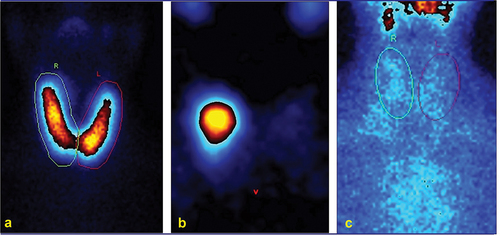
Figure 2. 99mTc-pertechnetate (a) and 99mTc-MIBI (b) scans: cold and MIBI active nodules in both lobes (arrows). Histopathology: multifocal invasive follicular variant of papillary thyroid carcinoma.
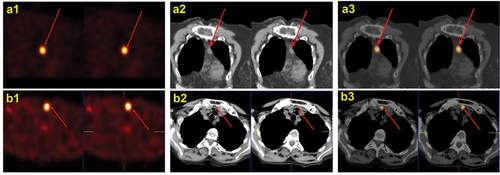
Figure 4. Post-ablation131I SPECT/CT (B) in a young female affected by papillary thyroid carcinoma (pT2 Nx) showing a central neck lymph-node metastasis.
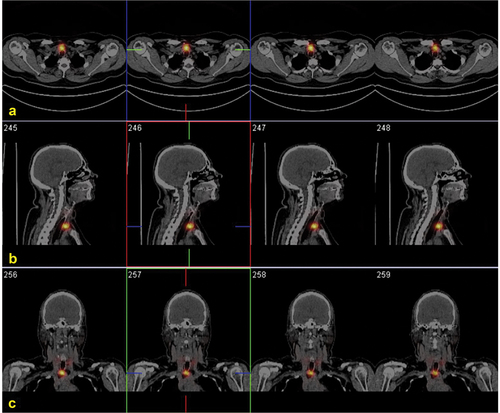
Figure 5. Post-therapy131I WBS (a, anterior; b, posterior views) and SPECT/CT (C) in a 50 years old female affected by papillary thyroid carcinoma (pT2 N1b) showing multiple visceral and skeletal radioiodine-avid metastases.
Figure 6. 18F-FDG PET maximum intensity projection image of a patient with poorly differentiated thyroid carcinoma showing increasing radiopharmaceutical uptake within the thyroid, corresponding to the primary tumor site and multiple lymph node, lung, liver, bone and renal metastases.

Figure 7. Parathyroid ultrasound: ovoidal hypoechoic nodule with vascular basket-pole, consistent with enlarged and hyperfunctioning parathyroid gland.
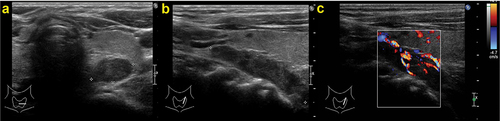
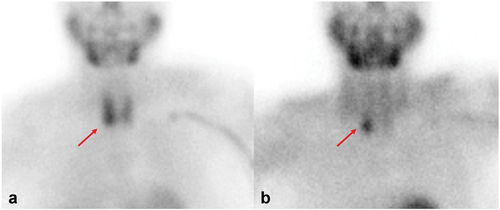
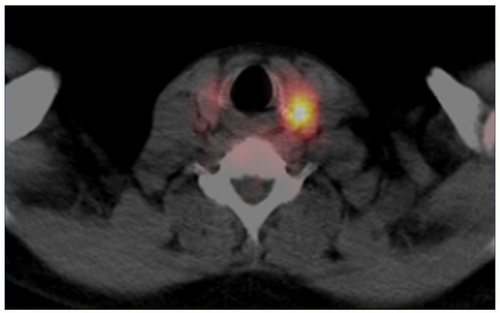
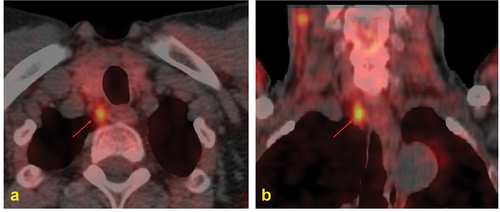
Figure 8. 99mTc-MIBI dual phase scintigraphy: tracer uptake and late retention in a parathyroid adenoma (red arrow).