Figures & data
Figure 1. Schematic structure of the dermal-epidermal junction. Only proteins that are targeted by autoantibodies in autoimmune blistering diseases are depicted.
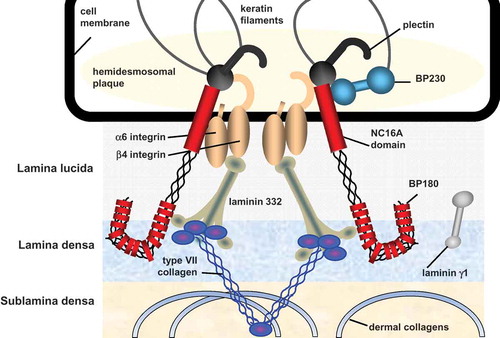
Figure 2. Structure of type VII collagen. CMP: cartillage matrix protein; 1–9: fibronectin III-like repeats 1–9; vWFA2: von Willebrand factor A; NC: noncollagenous.
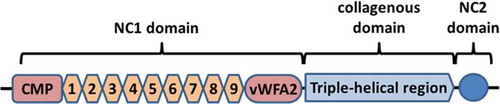
Figure 3. Classical variant of EBA. (a) Erythema and tense blisters on the right knee of a 6-year old boy. B. Erythema and erosions on the left hand of a 53-year old female.
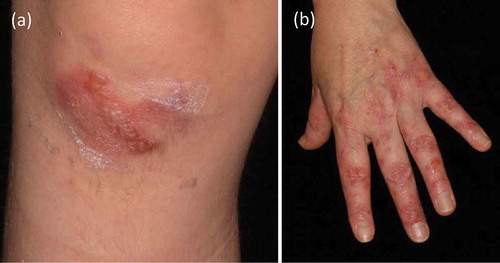
Figure 4. Inflammatory variant of EBA. (a) Erythema, erosions, and crusts on the left knee of a 76-year old patient. (b) Blisters and erosions on the right elbow of the same EBA patient.
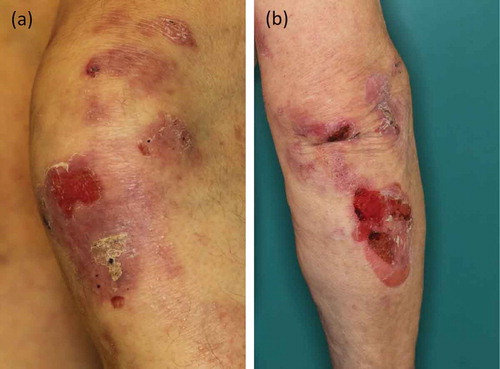
Figure 5. Mucosal involvement. (a) Blisters and erosions on the lower lip of a 6-year old boy (same patient as in . (b) Erosions on the tongue of a 76-year old male with EBA (same patient as in ,)
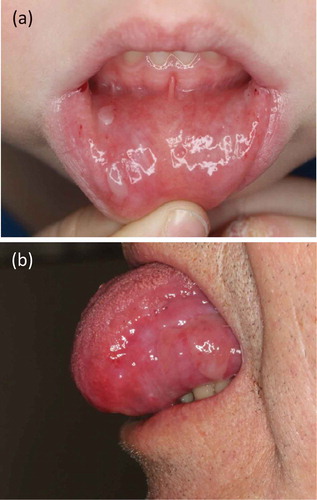
Figure 6. Direct immunofluorescence microscopy. (a) u-serrated deposition of IgG along the basement membrane zone in a patient with EBA. In contrast, in all of the pemphigoid diseases, an n-serrated pattern is seen, as exemplified in a patient with bullous pemphigoid (b). Magnification x 1000.
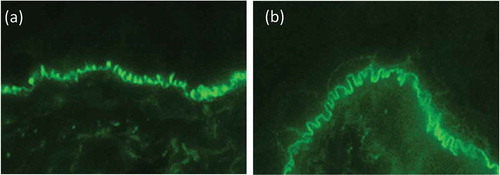
Figure 7. Indirect immunofluorescence microscopy. (a) Linear binding of IgG along the basement membrane on monkey esophagus. (b) IgG locates to the floor of the artificial blister in 1 M NaCl-split human skin.
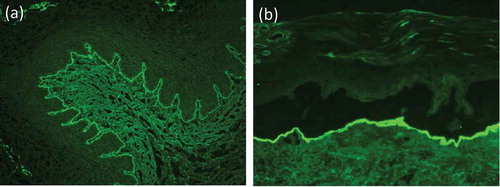
Figure 8. Indirect immunofluorescence on type VII collagen-deficient skin. Indirect immunofluorescence microscopy of a EBA patient’s serum on normal human skin shows linear labeling of IgG at the basement membrane zone (a), while on type VII collagen-deficient skin, no staining is seen (b; courtesy of Dr. Hendri Pas, Department of Dermatology, University of Groningen, The Netherlands).
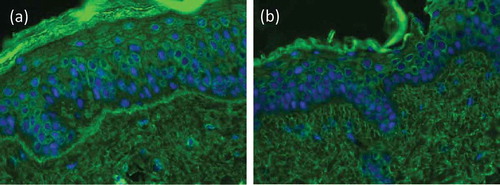
Figure 9. Western blotting. (a) Western blot with dermal extract. 1, blood donor; 2, positive control; 3, EBA patient; arrow indicates the migration position of type VII collagen. (b) Western blot with recombinant NC1 domain of type VII collagen. 1, blood donor; 2, positive control; 3, EBA patient; arrow indicates the migration position of NC1 domain.
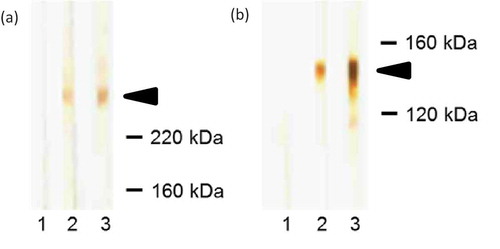
Figure 10. Correlation of serum levels of IgG antibodies against type VII collagen with disease severity. Serum autoantibody levels were detected by ELISA (diamonds; Euroimmun, Lübeck, Germany), disease activity was measured by a clinical score (triangles; 3, >10 lesions; 2, 4–10 lesions; 1, 1–3 lesions; 0, no lesions). Representative clinical pictures during the course of the disease are shown at the top.
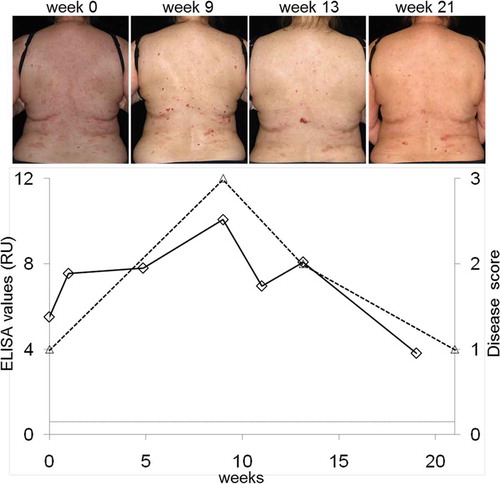
Figure 11. Indirect immunofluorescence on HEK 293 cells expressing the recombinant NC1 domain of type VII collagen on their cell surface.
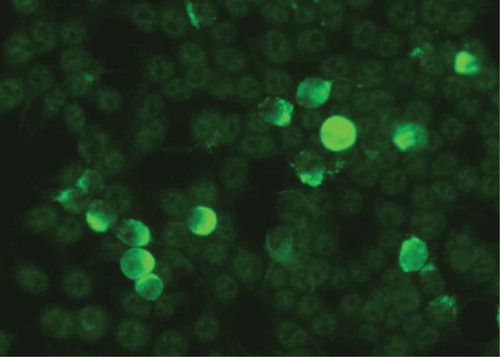
Figure 12. Diagnostic pathway for EBA.
1even when the diagnosis of EBA can be made based on an u-serrated pattern, detection of serum anti-type VII collagen antibodies is recommended; 2commercially available; 3depending of availability; positivity in any of the 4 assays will allow diagnosis of EBA; 4only available in specialized laboratories; 5from patients with dystrophic epidermolysis bullosa; 6bullous pemphigoid (BP), predominant IgG reactivity by direct and/or indirect IF microscopy, no floor binding by indirect IF microscopy, and no predominant mucosal involvement; mucous membrane pemphigoid (MMP), predominant mucosal involvement, when floor binding by indirect IF microscopy, laminin 332 reactivity needs to be analyzed; linear IgA diseases (LAD), predominant IgA reactivity by direct and/or indirect IF microscopy; anti-p200 pemphigoid, reactivity with the p200 protein and/or laminin γ1 [Citation4].
![Figure 12. Diagnostic pathway for EBA.1even when the diagnosis of EBA can be made based on an u-serrated pattern, detection of serum anti-type VII collagen antibodies is recommended; 2commercially available; 3depending of availability; positivity in any of the 4 assays will allow diagnosis of EBA; 4only available in specialized laboratories; 5from patients with dystrophic epidermolysis bullosa; 6bullous pemphigoid (BP), predominant IgG reactivity by direct and/or indirect IF microscopy, no floor binding by indirect IF microscopy, and no predominant mucosal involvement; mucous membrane pemphigoid (MMP), predominant mucosal involvement, when floor binding by indirect IF microscopy, laminin 332 reactivity needs to be analyzed; linear IgA diseases (LAD), predominant IgA reactivity by direct and/or indirect IF microscopy; anti-p200 pemphigoid, reactivity with the p200 protein and/or laminin γ1 [Citation4].](/cms/asset/04c2a00e-6ab4-4c9f-952f-eeda60049b08/ierm_a_1221343_f0012_oc.jpg)
