Figures & data
Figure 1. Inflammatory T2 pathway and mechanisms of action of Tezepelumab during chronic rhinosinusitis (CRS) and during chronic rhinosinusitis with nasal polyps (CRSwNP).
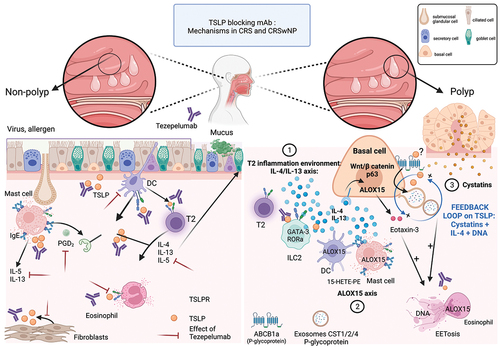
Table 1. Indirect evidence for TEZEPELUMAB efficacy in patients with CRSwNP.
