Figures & data
Table 1. Potential preoperative risk factors for failure of soft-tissue releases in 37 children, estimated as relative risks (RR) for failure, using Poisson loglinear regression
Figure 1. A. Preoperative radiograph of a 5 year 5-months-old boy with spastic quadriplegia (GMFCS level V), showing bilateral hip subluxation with migration percentage (MP) 40% (right hip) and 48% (left hip). B. 1.8 years after soft-tissue releases, showing good primary correction; MP of the left hip was reduced from 48% to 32%. C. 6.7 years postoperatively, showing good outcome with MP 15% (right hip) and 25% (left hip).

Figure 2. A.Preoperative radiograph of a 5 year 5 months old girl with spastic quadriplegia (GMFCS level V), showing subluxation of her left hip with migration percentage (MP) 50%. B. 1 year after soft-tissue releases, showing unsatisfactory primary correction; MP was reduced from 50% to 43%. C. 4.4 years postoperatively, showing poor outcome with MP 54% of the left hip. D. 3.1 years after Dega-type pelvic osteotomy and varus femoral osteotomy of the left hip (MP 31%).
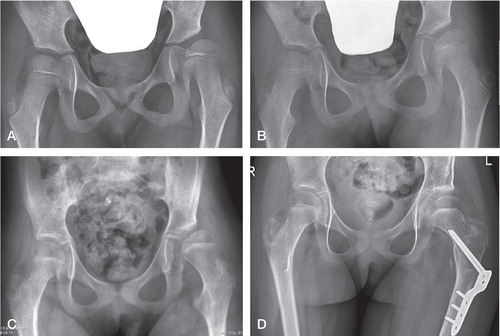
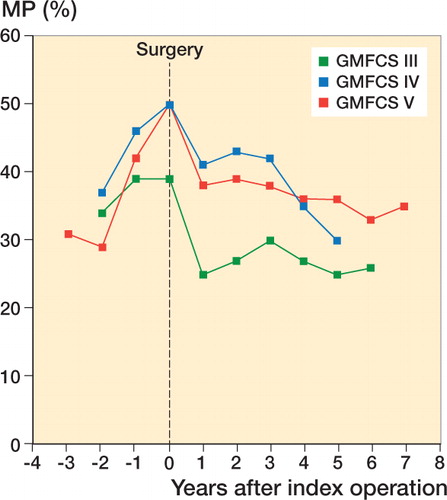
Table 2. Migration percentage (MP) pre- and postoperatively (mean MP of the worst hip in each patient) in 37 children and comparison between children with good and poor final radiographic results