Figures & data
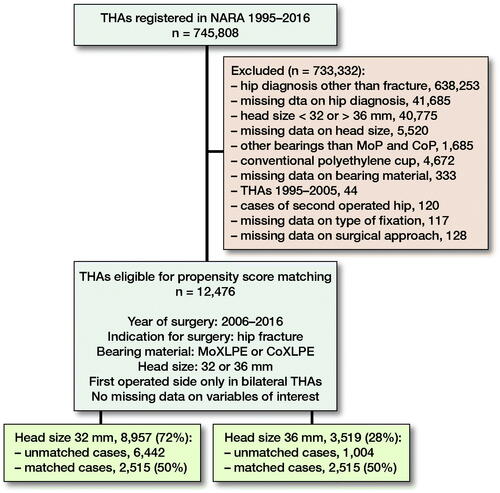
Figure 1. Use of 32- and 36-mm heads in MoXLPE and CoXLPE THA after proximal femur fracture in NARA database.
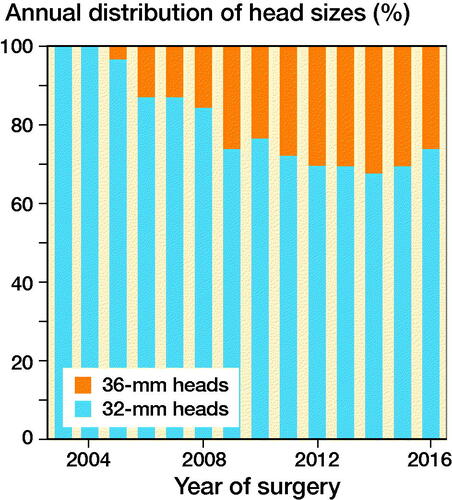
Figure 4. A directed acyclic graph (DAG) was constructed under the following assumptions:
1) THA ‘revision’ is dependent on ‘head size’, ‘patient age’, ‘sex’, ‘year of surgery’, surgical ‘approach’, and type of THA ‘fixation’. Choice of ‘head material’ is not expected to affect ‘revision’ due to the short follow-up of the study.
2) Choice of ‘head size’ is dependent on ‘approach’, ‘year of surgery’, ‘sex’, and ‘patient age’ as surgeons operating on older patients through a posterior approach have presumably chosen a larger head in order to, hopefully, reduce the risk of dislocation. Male patients, operated more recently, have probably received a larger head due to their larger acetabulum and because the use of larger heads has become more popular with time.
3) ‘Fixation’ is dependent on ‘year of surgery’ and ‘age’ because patients operated more recently have probably received an uncemented THA, due to the popularization of this technique, and older patients have probably received a cemented THA due to their poorer bone quality.
4) ‘Head material’ is dependent on ‘head size’ and ‘patient age’ because surgeons have probably chosen ceramic over metal heads in younger patients and when choosing larger heads due to the presumed lower polyethylene wear.
Provided that our assumptions are correct, adjusting for ‘patient age’, ‘sex’, ‘year of surgery’, and ‘approach’ in the multivariable Cox regression model should block all backdoor pathways (for variables available in our database) confounding the effect of ‘head size’ on ‘revision’.
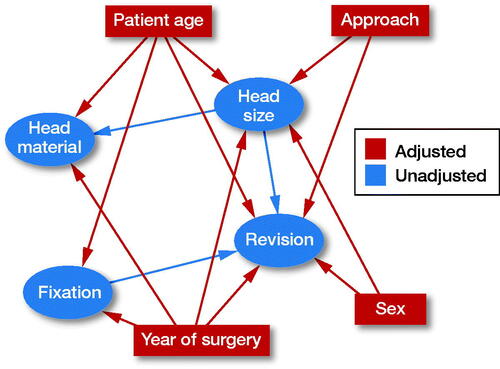
Table 2. Descriptive statistics of study population after propensity score matching. Values number (%) unless otherwise specified
Table 1. Descriptive statistics of study population before propensity score matching. Values number (%) unless otherwise specified
Figure 5. Kaplan–Meier survival function for THA with 32- and 36-mm heads with endpoint revision for any reason (left panel) and revision due to dislocation (right panel).
Table 4. Cox proportional hazards models with endpoint revision for any reason and due to dislocation
Table 3. Kaplan–Meier survival estimates (%) at 1, 3, and 7 years for 32- and 36-mm heads with endpoint revision for any reason
Table 5. Kaplan–Meier survival estimates (%) at 1, 3, and 7 years for 32- and 36-mm heads with endpoint revision due to dislocation