Figures & data
Table 1. Efficacy outcomes and reported serious adverse events (SAE) for the seven published randomized controlled trials using valves for emphysema. * follow -up: 0–30 days and 30 days – 6 months; # follow -up: 0–45 days and 45 days – 12 months; $ follow -up: 0–6 months and 6–12 months. Abbreviations: SVS: Spiration Valve System; EBV: Endobronchial valves; FEV1: Forced Expiratory Volume in the first second; RV: Residual Volume; SGRQ: St George’s Respiratory Questionnaire; 6MWD: 6 minute walking distance
Figure 1. Example of an incomplete occlusion of the lingula. (a): LB4 (red arrow) and LB5 (blue arrow) before treatment. (b): The EBV was supposed to occlude both segments, but occluded only LB4, thus preventing the occurrence of a full lobar atelectasis
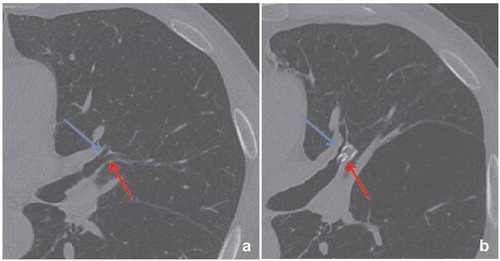
Figure 2. Bronchial angulation of the non-treated lobe left lower lobe. The red arrows indicate the airways before (a and c) and after (b and d) treatment, and shows the folding of the airway of the left lower lobe. Abbreviations: LUL; Left Upper Lobe, LLL; Left Lower Lobe
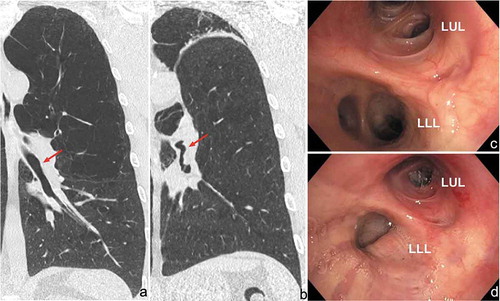
Figure 3. Images of thorax CT scan showing valve migration. In this case, the left lower lobe was treated with endobronchial valves and 6 weeks after treatment a complete atelectasis of the target lobe was achieved with a significant clinical benefit. After six months, there was loss of clinical benefit and no more lung volume reduction. (a): EBV well positioned in LB6. (b): Complete re-expansion of the treated lobe, the valve in LB6 is dislocated and now in a different position compared to the follow-up scan at six weeks
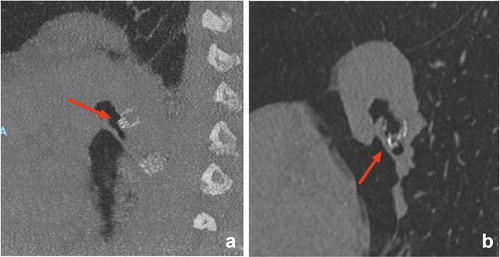
Figure 4. Malfunction of EBV due to mucus impaction. The valve mechanism is compromised and constant flow over the valve prevents target lobe volume reduction

Figure 5. Loss of effect due to valve dislocation which causes leakage along the Spiration Valve System (a) and Endobronchial Valve (b)
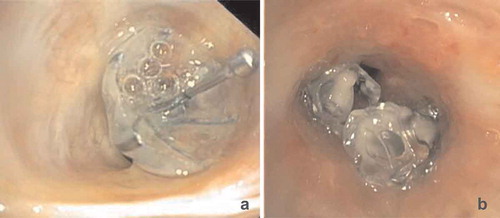
Figure 6. Migration of EBV to the contralateral lung. Endobronchial valves were placed into the left lower lobe resulting in a complete atelectasis and clinical benefit. One year after the treatment, the patient presented with complaints of progressive dyspnea. (a): The CT-scan showed migration of a valve from the left lower lobe to the right lower lobe, the arrows indicate the position of the valves on both sides. (b): The valve in the entrance of the non-target right lower lobe in reversed position. (c): Endoscopic image of the valve position in reversed position, which was removed and replaced by a new valve in the original left lower lobe position
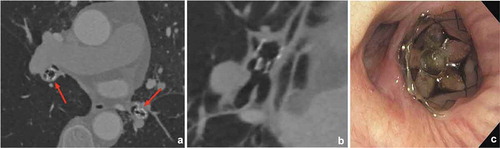
Figure 7. Endoscopic images showing granulation tissue in the segmental airways. (a): RB3 (anterior segment of the right upper lobe) before treatment. B: Same segment (RB3), after removal of the valve, which shows an extensive granulation reaction behind the valve. (c): RB3 and RB2 (posterior segment of the right upper lobe) directly after placement of EBVs. (d): Same position as in C with granulation tissue. E: Endobronchial view of an SVS directly after placement. (f): Endobronchial view of the SVS being displaced with granulation tissue formation
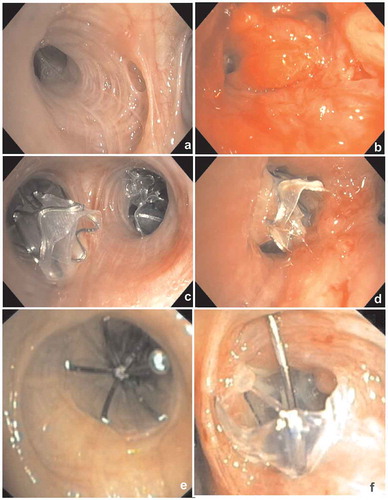
Figure 8. (a): Pneumothorax 1 day after treatment with endobronchial valves in the left upper lobe (indicated by arrows). There is a mediastinal shift to the right, indicating volume expansion due to the pneumothorax. This patient was treated with a chest tube only. (b): Pneumothorax ex vacuo (indicated by arrows) 1 day after treatment with endobronchial valves in the right upper lobe, the pneumothorax resolved spontaneously. Note: there is still volume loss on the site of the pneumothorax. (c and d): Extensive subcutaneous emphysema and pneumomediastinum due to a large air leak after treatment of the left lower lobe. This patient was successfully treated with surgical bullectomy to treat the air leak
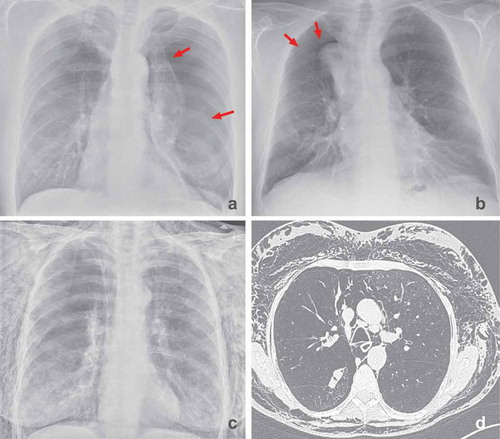
Figure 9. This patient was successfully treated with endobronchial valves in the left lower lobe. Two years later the patient presented with a postobstruction pneumonia. (a): The CT-scan showed an increased volume of the atelectasis of the left lower lobe. (b): After treatment with antibiotics and removal of two of the valves, there was clinical improvement and partial resolution of the consolidation. Due to the important initial clinical benefit of the valve treatment, this patient was treated by VATS lobectomy after full recovery of the pneumonia, rather than removal of the valves and experienced persistent clinical benefit
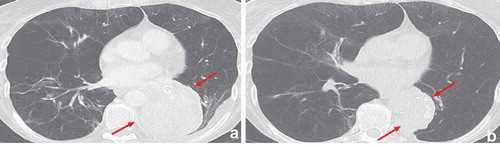
Figure 10. Airway ulceration due to contact of the valve with the opposite airway wall which led to hemoptysis. In this case valve removal was sufficient to treat the hemoptysis

