Figures & data
Figure 1. Photographs of the transfer support device “Hug” and its mechanism of action. Photographs of Hug (A) and an example of the use of Hug (B). After placing the care recipient in the correct position (C), pressing the “Stand up” button moves the centre of gravity of the care recipient’s chest (closed green circles) horizontally and also raises their buttocks (D). Next, the robotic arms rotate and the shaft rises further, causing the care recipient to stand up (E). The angle of the robotic arms is shown by yellow lines, the green lines show the movement of the care recipient, and the thin broken lines show the horizontal level. The images in A and B were kindly provided by Fuji Corporation with permission for use in publications.
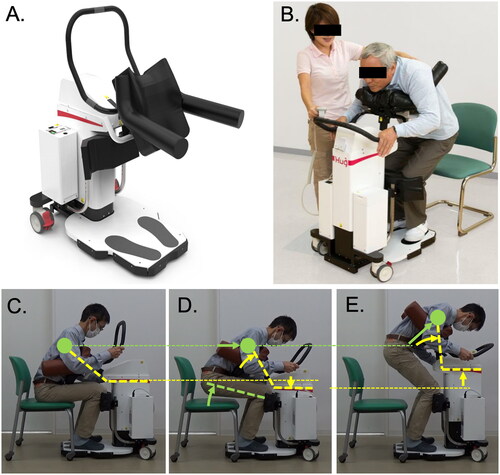
Table 1. Information about the target care recipients of Hug.
Figure 2. Time involved in transfers using Hug during the development of proficiency after its introduction. The transfer time using Hug at the unskilled facility, which was 4.6 min on average in the second week after introduction, was reduced to 3.0 min on average in the fifth week after introduction. And the transfer time at the skilled facility was 1.5 min on average. The results were obtained from the time study performed in Measurement Period 1, as described in the Methods section.
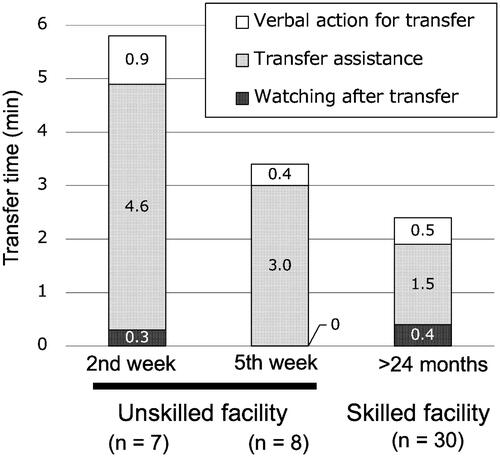
Figure 3. Changes in the number of transfers with or without Hug before and after its introduction. The numbers in the unskilled facility were compared with that in the skilled facility. The frequency of Hug use in the unskilled facility increased slowly, even after 5 weeks of use, it did not reach 50% of transfers; however, the number of transfers with multiple assistance decreased significantly to 3.5 out of 29.5 transfers/person/week. In contrast, skilled facilities used Hug for most transfers. The results were obtained from Measurement Period 1.
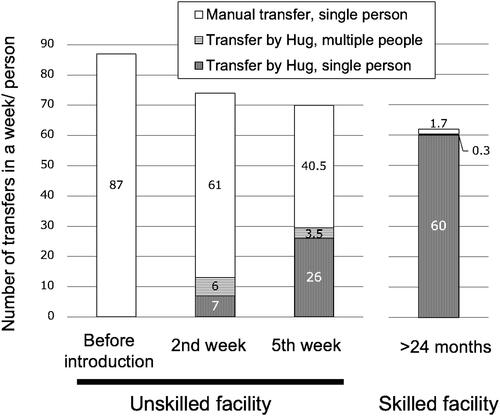
Figure 4. Results of the questionnaire before and after the introduction of Hug. Comparing the results at the unskilled facility (before introduction and using Hug for 6 weeks) and at the skilled facility (using Hug >24 months). Questions: (A) “Was physical burden reduced by the use of Hug?” (B) “Did you have sufficient mental capacity when performing transfers using Hug?” and (C) “Was communication with the care recipient increased by the use of Hug?” In the case before the introduction of Hug to the unskilled facilities, the questions were changed to A, “Do you expect that the use of Hug will reduce physical burden?” B, “Do you expect to have sufficient mental capacity when performing transfers using Hug?” and C, “Do you expect that communication with the care recipient will be increased by the use of Hug?” Questionnaire forms are attached as Supplementary figures 3 & 4.
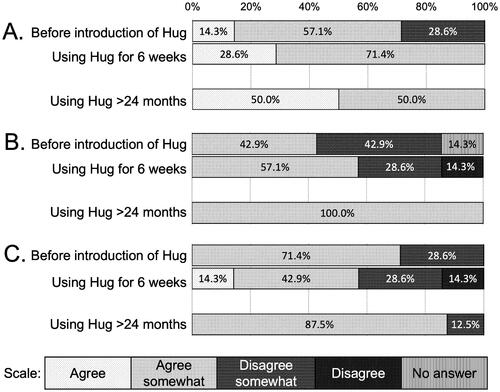
Table 2. Assessment correspondence chart for target care recipients.
Supplementary_Materials.pdf
Download PDF (561.3 KB)Data availability and materials
The datasets analysed during the current study are not publicly available given that the research team has not completed its analysis, but are available from the corresponding author on reasonable request.
