Figures & data
Figure 1. Gut microbiota and cardiovascular disease. Various gut microbiota in the human body, such as Streptococcus, staphylococcus and Helicobacter pylori, can activate neutrophils in various ways to cause inflammatory reaction, thus causing excessive ROS accumulation in the body and damaging mitochondrial function; on the other hand, SCFAs produced by gut microbiota ingesting dietary components can also trigger autophagy through PI3K/Akt/mTOR pathway. The above mechanisms play a key role in age-related cardiovascular diseases such as atherosclerosis, hypertension, myocardial infarction, myocardial hypertrophy and fibrosis. (ROS: reactive oxygen species. SCFAs: short-chain fatty acids).
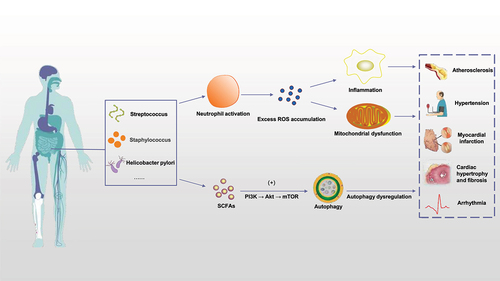
Figure 2. Mitochondrial dysfunction affects the underlying mechanisms of age-related cardiovascular disease. TMAO can promote mitochondrial DNA mutation, thus affecting OXPHOS, increasing ROS production, decreasing ATP/ADP ratio, further damaging mitochondrial DNA, and causing impaired calcium ion metabolism, intracellular calcium overload, and promoting cell apoptosis. Increased oxidative stress activates AMPK, which activates autophagy and degrades damaged mitochondria. (TMAO: trimethylamine N-oxide. OXPHOS: oxidative phosphorylation. AMPK: AMP-activated protein kinase).
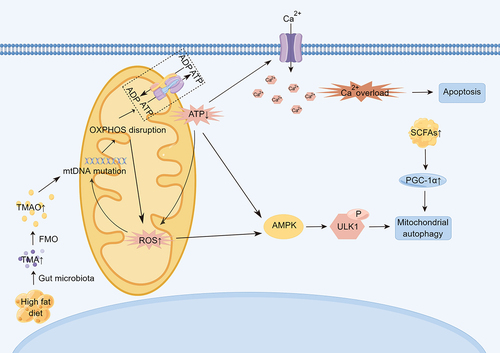
Figure 3. Gut microbiota and aging. The composition of intestinal flora and the level of derived metabolites changed with age. The composition and function of an infant’s early microbiota are influenced by factors such as birth mode and early feeding pattern, and the gut microbiota is influenced by more factors such as genetics, diet, mood, and life events as the infant ages. However, the general trend was that with the increase of age, the diversity of intestinal flora increased, the number of Bacteroides decreased significantly, and the number of Firmicutes increased, the level of TMAO increased, and the abundance of SCFAs producing bacteria decreased. However, due to the existence of higher inflammation levels in centenarians, the diversity of intestinal flora decreased, the proportion of Firmicutes decreased, and Bacteroides increased. (TMAO: trimethylamine N-oxide. SCFAs: short-chain fatty acids).
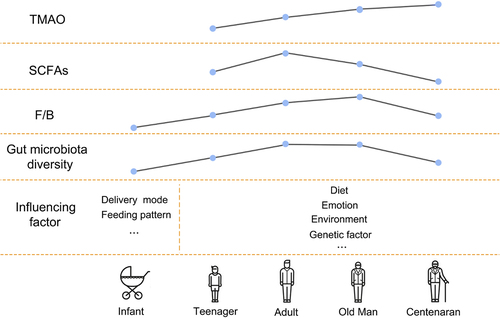
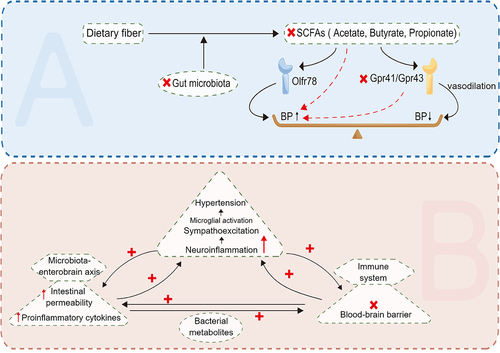
Figure 4. The relationship between hypertension and SCFAs and neuroinflammation. SCFAs increases blood pressure through Olfr78, and also acts on Gpr41 and Gpr43, promoting vasodilation and thus lowering blood pressure. At the same time, neuroinflammation and activity imbalance of autonomic nervous system caused by gut-brain axis dysfunction can also lead to elevated blood pressure. (SCFAs: short-chain fatty acids).
Data availability statement
The data used to support the findings of this study are included within the article.
