Figures & data
Figure 1. The manifestations and pathophysiology of chronic urticaria.

Table 1. A summary of current evidence on the association between gut microbiome composition and chronic urticaria (mainly CSU).
Figure 2. The alteration and influence of gut microbiome in chronic urticaria.
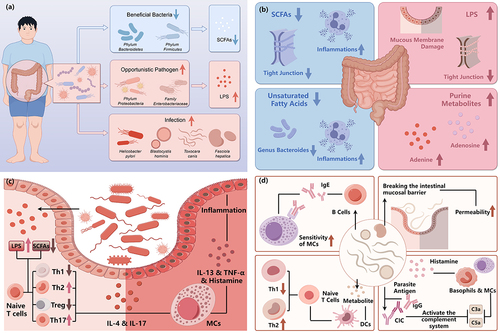
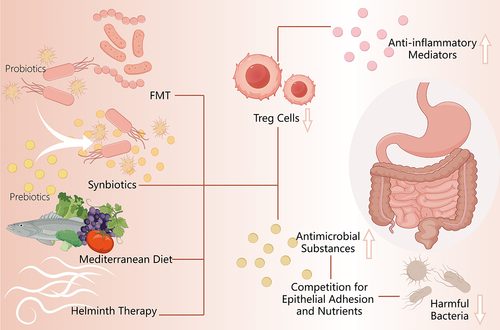
Figure 3. Summary of relevant therapies of chronic urticaria targeted at gut microbiome.