Figures & data
Table 1. Antiseizure medications.
Table 2. Baseline demographic and clinical characteristics of commercial/Medicare Supplemental patients.
Table 3. Baseline demographic and clinical characteristics of Medicaid patients.
Figure 1. Non-mutually exclusive sample attrition commercial and medicare patients.
Notes: AED – antiepileptic drug. a Continuous enrollment could only be verified for patients with an AED prescription fill within the enrollment window, as only these patients were assigned an index date. b Not mutually exclusive.
Table 4. Baseline healthcare utilization of commercial/Medicare Supplemental patients and Medicaid patients.
Table 5. Baseline healthcare costs of commercial/Medicare Supplemental patients and Medicaid patients.
Table 6. Treatment patterns of commercial/Medicare Supplemental patients and Medicaid patients.
Table 7. Pre-index and post-index healthcare costs among clobazam patients in the commercial/Medicare Supplemental and Medicaid populations.
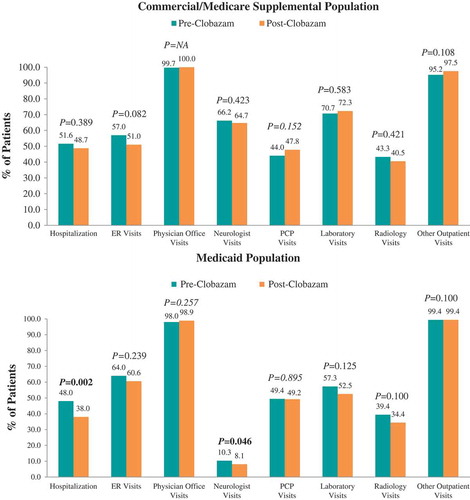
Figure 2. Proportion of patients utilizing seizure-related healthcare resources pre- vs post-clobazam.
Notes: ER – emergency room; PCP – primary care physician. P-values in bold < 0.05. P-values for unadjusted differences in categorical variables were obtained using McNemar’s test to account for pre-post design.
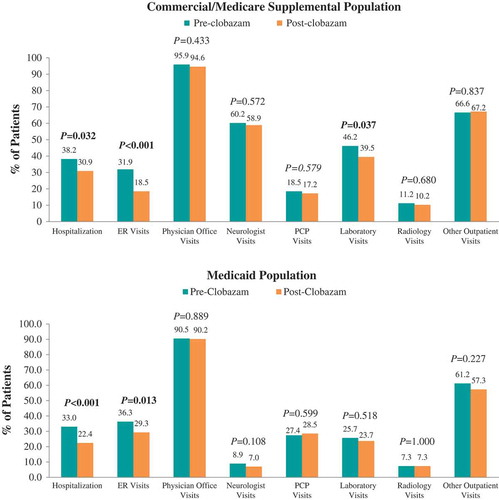
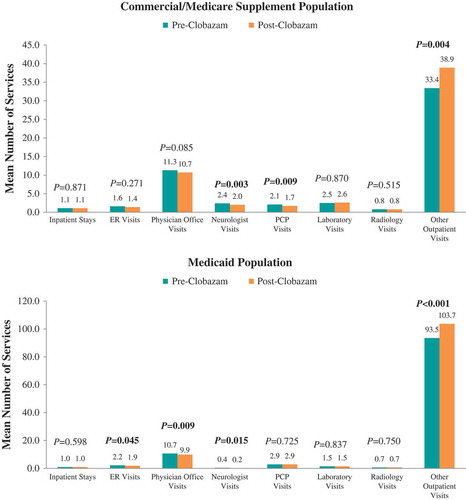
Figure 3. Mean number of seizure-related healthcare services utilized pre- vs post-clobazam.
Notes: AED – antiepileptic drug; ER – emergency room; PCP – primary care physician. P-values in bold < 0.05. P-values for count variables were obtained using paired t-tests to account for pre-post design. *Includes clobazam.
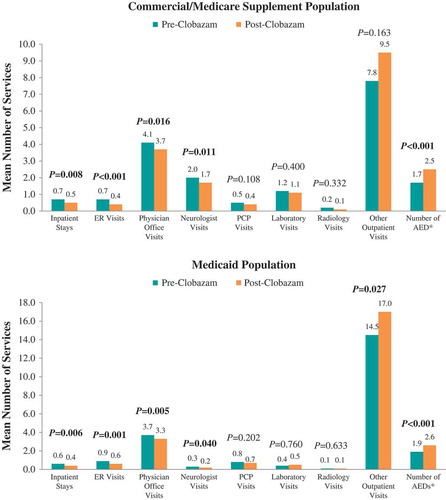
Figure 4. Proportion of patients utilizing all-cause healthcare resources pre- vs post-clobazam.
Notes: ER – emergency room; PCP – primary care physician. P-values in bold < 0.05. P-values for unadjusted differences in categorical variables were obtained using McNemar’s test to account for pre-post design.