Figures & data
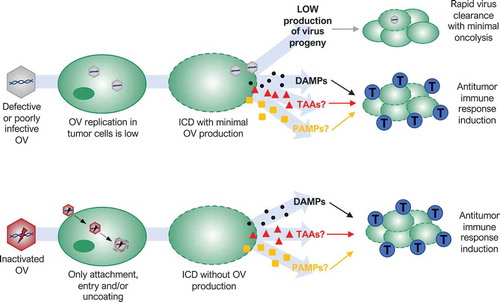
Figure 1. Dual-mode of action of oncolytic viruses (OVs). OVs preferentially target and kill cancer cells while having minimal to no detrimental effects on normal cells. OVs mediate tumor cell destruction by two main mechanisms: direct lysis of infected cells (oncolysis) and indirect augmentation of host antitumor immunity. OVs infect and replicate in cancer cells, inducing tumor cell lysis and release infectious viral progeny that spreads to surrounding tumor cells (amplification of oncolysis). Oncolysis also releases tumor-associated antigens (TAAs), cellular damage-associated molecular patterns (DAMPs) and pathogen-associated molecular patterns (PAMPs) in a highly inflammatory process, termed “immunogenic cell death” (ICD). Cellular detection of viral infection and the products of oncolysis trigger the rapid activation of a host antitumor immune response. The direct recognition and killing of tumor cells are primarily mediated by natural killer cells of the innate immune system and tumor antigen-specific CD8+ cytotoxic T lymphocytes (blue cells) of the adaptive immune system.
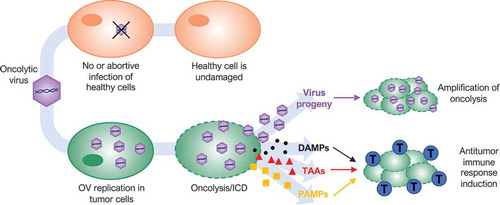
Figure 2. Possible mechanisms of action of oncolytic viruses (OVs) that oppose traditional dogma that correlates replication with efficacy. Defective or poorly infective OVs may produce a small amount of new viral particles after infection of tumor cells, but infection spreading is quickly stopped by a host antiviral response (rapid virus clearance with minimal oncolysis). Nevertheless, several defective, poorly infective or even inactivated OVs are able to kill tumor cells in an immunogenic way. Low virus replication or only virus binding, entry and/or uncoating in tumor cells are enough to induce immunogenic cell death (ICD) releasing damage-associated molecular patterns (DAMPs) that triggers a host antitumor immune response activation or augmentation (blue cells: cytotoxic T lymphocytes). Whether tumor-associated antigens (TAAs) or pathogen-associated molecular patterns (PAMPs) are also involved remains unknown.