Figures & data
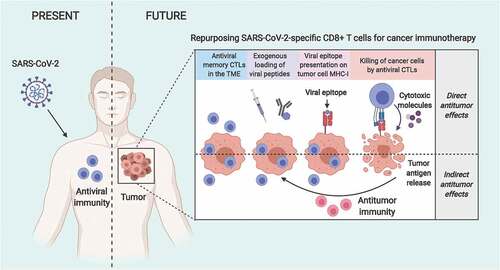
Figure 1. Repurposing SARS-CoV-2-specific antiviral CD8+ T cells for cancer immunotherapy. Patients recovered from COVID-19 or immunized with the relevant vaccines are expected to develop CD8+ T cell immunity against SARS-CoV-2. Tumors developing later on in SARS-CoV-2-immunity-bearing individuals will likely host SARS-CoV-2-specific CD8+ T cells that could be repurposed to target cancer cells. In this therapeutic approach, delivery of SARS-CoV-2-derived immunogenic epitopes (via, for example, adjuvant-free intratumoral injection or antibody-peptide epitope conjugatesCitation9,Citation10) results in their presentation by MHC-I molecules on the surface of cancer cells. Consequently, antiviral CD8+ T cells recognize their cognate epitopes and get ‘tricked’ into killing these cancer cells, simulating a virus infection (direct antitumor benefits of antiviral CD8+ T cells). Additionally, the spreading of tumor antigens released during the initial direct killing by antiviral CD8+ T cells facilitates their cross-presentation by APCs and the induction of an antitumor immunity that will attack any residual or recurring cancer cells (indirect antitumor benefits of antiviral CD8+ T cells). Interestingly, the antitumor benefits of such antiviral CD8+ T cell repurposing approaches can be further potentiated with immune checkpoint inhibitors. CTL, cytotoxic CD8+ T lymphocyte; MHC-I, major histocompatibility complex class-I; TME, tumor microenvironment.