Figures & data
Figure 1. Immunosenescence affects various immune cell functions in response to infection or vaccination. Functions that are reduced due to immunosenescence are indicated by red downward arrows, increased functions are represented by red upward arrows, conserved functions are denoted by green circles with a “C” inside, and functions with unclear changes are marked by black circles with question marks. Inflammaging, characterized by heightened basal inflammation, leads to decreased activation of immune cells. Specifically, CD28 expression on T cells decreases due to the inflammaging. While many functions of dendritic cells (DCs) decline with immunosenescence, the functions of TLR2 and TLR4 are conserved, and NLRP3 functions are increased. Reduced expression and signaling of TLRs, exposure to chronic inflammation, and decreased co-stimulator expression levels of DCs impact the impaired functions of B and T cells. T cells show reduced functionality due to immunosenescence. Decreased co-stimulator expression on DCs and reduced CD28 expression on T cells result in diminished T cell activation. An increased TCR threshold leads to reduced TCR signaling, and a decreased TCR repertoire contributes to the decline in T cell function. A reduced BCR repertoire and decreased BCR signaling negatively affect antigen recognition and differentiation functions of B cells. In particular, decreased CD40L expression on CD4 T cells and reduced CD40 expression on B cells induce diminished activation of B cells, leading to a reduction in antibody production in response to vaccines. These functional declines in DCs, B, and T cells, result in reduced immune responses, making the elderly more susceptible to infections and diminishing the effectiveness of vaccines. Abbreviations: DCs, dendritic cells; TLR, toll-like receptor; NLRP3, nucleotide-binding oligomerization domain (NOD)-like receptor family pyrin domain-containing 3; TCR, T cell receptor; BCR, B cell receptor.
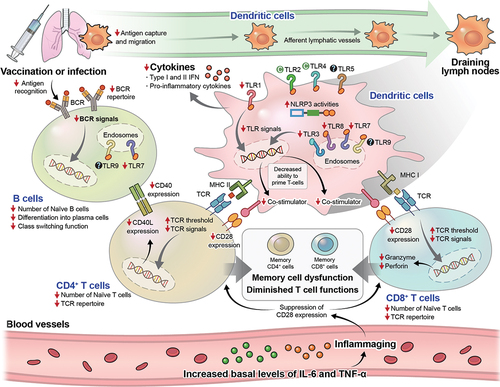
Table 1. The number of kinds of adjuvants used in vaccines currently under developments for major diseases affecting the elderly (Varicella-zoster virus, VZV; Influenza A; Streptococcus pneumoniae, S. pneumoniae) [Citation22], emerging antibiotic resistance threats (Clostridioides difficile, C. difficile; Neisseria gonorrhoeae, N. gonorrhoeae; Klebsiella pneumoniae, K. pneumoniae; Shigella sp.) [Citation26], and pathogens under active vaccine research (Respiratory Syncytial Virus; RSV, Hepatitis B virus, HBV, Mycobacterium tuberculosis, Mtb; SARS-CoV-2) [Citation29, Citation47, Citation281] are classified based on their target PRRs. The numbers listed in the table represent the number of types of adjuvants classified based on the targeting Toll-like receptors and immune profiles. Please note that there was no information available on adjuvant developments associated with Acinetobacter baumannii, Candida auris, and Enterobacteriaceae, despite their listing as emerging antibiotic resistance threats by the Centers for Disease Control and Prevention. (https://vac.niaid.nih.gov/, last accessed on January 20, 2024).
Figure 2. TLR activation pathways. TLRs play a crucial role in the recognition of microbial components and the initiation of immune responses. TLR1, TLR2, TLR4, TLR5, and TLR6 are expressed on the cell surface, where they primarily recognize microbe-derived lipopeptides, peptidoglycan, lipopolysaccharide (LPS), and flagellin, leading to inflammatory responses. TLR1 and TLR6 form heterodimers with TLR2 to execute their functions. TLR3, TLR7, TLR8, and TLR9 are located in intracellular vesicles, where they recognize dsRNA, ssRNA, and CpG DNA. MyD88 is a common signaling molecule utilized by all TLRs except TLR3. TLR3 uses TRIF as its signal transducer. TLR4 signaling molecule changes from MyD88 to TRIF once TLR4 relocates to endosomes. Upon binding to TLR ligands, MyD88 becomes activated, leading to the formation of the myddosome. Subsequently, the TAK1 complex and IKK complex are activated, which induces NF-κB. Activation of MyD88 by TLR2 results in the activation of MAPKs, leading to the activation of ERK. This, in turn, results in the induction of cFos protein and the activation of the transcription factor AP1. Activation of MyD88 by TLR7, TLR8, and TLR9 ligand binding can directly induce IRF7. TLR3 and TLR4 activation through TRIF leads to the induction of TRAF6 and TRAF3. TRAF3 activates TBK1 and IKKi and induces the transcription factor IRF3. Additionally, TRAF6 can activate TAK1 and IKK. Activation of various TLRs results in the activation of specific transcription factors, which influence the immune profile. Transcription factor AP1 promotes Th2-biased immune responses by stimulating the production of anti-inflammatory cytokines. NF-κB promotes the secretion of pro-inflammatory cytokines, inducing Th1-biased immune responses. Transcription factors IRF3 and IRF7 promote the secretion of type I IFN cytokines, along with the activation of CTL, contributing to Th1-biased immune responses. Abbreviations: TLR, toll-like receptor; ssRNA, double-stranded RNA; MyD88, myeloid differentiation factor 88; TRIF, TIR domain-containing adapter-inducing interferon-β; TAK1, transforming growth factor-β-activated kinase 1; IKK, IκB kinase; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; MAPKs, mitogen-activated protein kinases; ERK, extracellular signal-regulated kinase; AP1, dimeric transcription factor complex activator protein-1; IRF, induce interferon regulatory factor; TRAF, TNF receptor-associated factor; TBK, TANK-binding kinase; CTL, cytotoxic T lymphocytes.
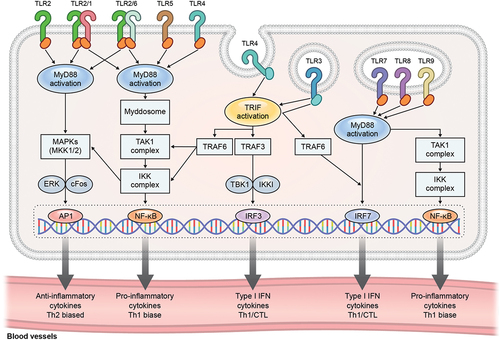
Table 2. The characteristics of adjuvants and their application in clinical development against infectious diseases.
