Figures & data
Table 1 Seven questions in the survey were aimed at determining individual practice in genetic testing in patients with apparently sporadic disease.
Figure 1 Current practice in genetic testing of apparently sporadic ALS in the UK as surveyed from 30 clinicians in 21 ALS care centers. (A) Classification of ALS into familial or sporadic disease remains variable with 57% (17/30) of clinicians considering that a family history (FH) of ‘uncharacterised dementia’ is not equivalent to a FH of FTD, whilst 43% (13/30) considered it equivalent. Additional comments, provided in Supplementary File 2, further highlight the lack of consensus and inherent variability in the classification of ALS into apparently sporadic or familial. (B) The majority of clinicians feel comfortable discussing genetic testing in ALS 70% (21/30); 27% (8/30) feel somewhat uncomfortable and 3% (1/30) very uncomfortable. (C) 47% (14/30) of clinicians discuss monogenic disease etiology with all newly diagnosed patients, 40% (12/30) do so on selected cases when certain factors suggest possible genetic etiology, 10% (3/30) only when the patient or relatives raise the topic and 3% (1/10) avoid the discussion. (D) The majority of clinicians (47%; 14/30) offer genetic testing to patients on selected cases when monogenic disease etiology is suspected, 27% (8/30) offer testing routinely to patients diagnosed with apparently sporadic disease and 13% (4/30) refer the patient to a different service, even if they had a discussion on the genetic etiology of ALS. Of the 13% (4/30) of respondents who took alternative action ("other"), 2/4 clarified that they do not refer as this would be a decision for the consultant in clinic, 1/4 commented that their practice in regard to accessing genetic testing was constrained due to commissioning arrangements and 1/4 reported that they would perform the test but subsequently refer to local or regional genetics services if the genetic test was positive (see free text comments Supplementary File 2).
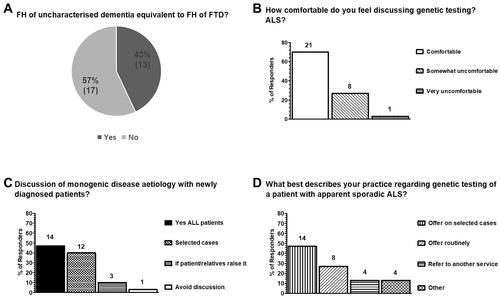
Figure 2 Current views on which setting genetic testing for ALS should be conducted and whether it is now time to test all patients with apparently sporadic disease in the UK as surveyed from 30 clinicians in 21 ALS care centers. (A) 67% (20/30) of clinicians considered that testing should be performed in the ALS services and, additionally, clinical genetics services. 23% (7/30) were of the opinion that genetic testing can be performed in the context of a general neurology clinic, or an ALS or clinical genetics service and 10% (3/30) considered that testing should only take place in the ALS services. (B) In regard to genetic testing, when a patient is diagnosed outside the ALS services or the ALS clinician is uncomfortable discussing genetic testing, 50% (15/30) of respondents considered that the best action is to refer patients to clinical genetics, 47% (14/30) to a different ALS care centre with expertise in genetics and 3% (1/10) considered that sending the genetic test at the patient’s request is the most appropriate action. (C) The majority of clinicians (77%; 23/30) considered that, at present, it is not appropriate to offer genetic testing to all patients diagnosed as apparently sporadic ALS routinely. 20% (6/30) considered that all patients diagnosed with apparently sporadic disease should now be offered testing and 3% (1/30) were unsure.
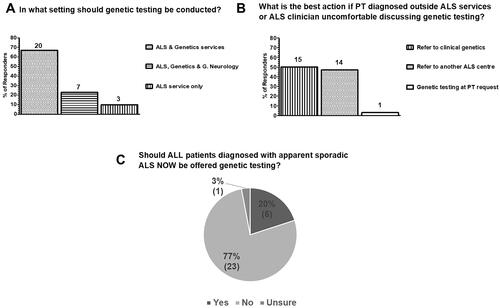
Table 2 Three questions were aimed at determining individual practice in genetic testing in asymptomatic/pre-symptomatic at-risk relatives of patients with monogenic MND/ALS.
Figure 3 Current practice in genetic testing and counseling services for pre-symptomatic relatives of patients with monogenic ALS (at-risk individuals) and pre-symptomatic carriers in the UK as surveyed from 30 clinicians in 21 ALS care centers. (A) Genetic testing for asymptomatic/pre-symptomatic relatives of patients with monogenic disease is only offered by 27% (8/30) clinicians, whilst 73% (22/30) do not offer this service. (B) 57% (17/30) of respondents reported having an onward referral pathway for pre-symptomatic pathogenic variant carriers for pre-conception advice whilst 43% (13/30) reported not having an onward referral pathway for this purpose. (C) Most clinicians have never referred a patient carrying an ALS pathogenic variant for pre-conception counseling (57%; 17/30), 20% (6/30) were not able to answer and only 23% (7/30) have referred patients for pre-conception counselling (6/7 between 1 and 5 patients and 1/7 5 patients).
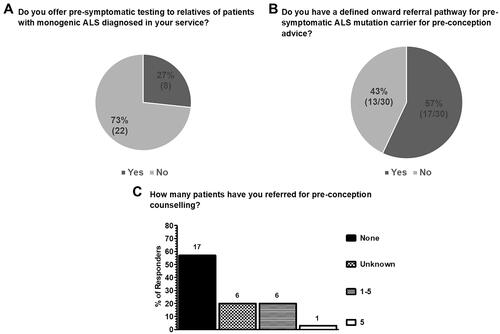
Table 3 Tabulated answers for each respondent, in each care centre (care centre 1-21; CC1-CC21) to the question “Do you have a defined onward referral pathway (even if not written as a protocol) for pre-symptomatic MND/ALS pathogenic variant carriers for pre-conception advice?”.
Supplemental Material
Download PDF (96.2 KB)Supplemental Material
Download MS Word (21 KB)Data availability statement
The data that support the findings of this study are available in this article and its supplementary files in an anonymised format. Individualized data are not publicly available due to their containing information that could compromise the privacy and anonymity of research participants.
