Figures & data
Table 1. Patient characteristics at baseline.
Table 2. Feasibility of pTULSA.
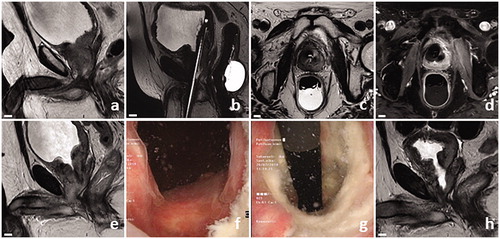
Figure 2. Successful pTULSA case example. Patient presented with radio recurrent castration-resistant LAPCa (rT4N1M1b, GGG5, PSA 19), was continuously catheterized, had a history of recurrent gross hematuria, and the prostatic urothelium line was bleeding from cystoscopy contact. Baseline sagittal MRI image showed obstructive infiltration of PCa to the bladder neck and posterior bladder wall (a). Treatment-day MRI planning images showing the transurethral ultrasound applicator and endorectal cooling device (b and c). 19 cc of tumor around the bladder neck was targeted, with contrast-enhanced MRI revealing immediate effects of ablation (d). Transurethral catheter removal was successful at 1 week, accompanied with a prostate volume increase from 35 to 40 cc on MRI (e). Cystoscopy revealed an open bladder neck at 3 months (f and g). A clear cavity could be seen around the proximal prostatic urethra on MRI, with a corresponding decrease in prostate volume to 12 cc at 12 months (h).