Figures & data
Figure 1. Schematic of electrolyte transporters and junctional proteins in IECs: Ion transporters, channels, physical and chemical barriers are compromised in IBD leading to diarrhea. The transepithelial pathway of solutes and ions is mediated by ion/solute transporters and channels. As depicted in the figure, in steady state, apical transporters, NHE3 (Na+/H+ exchanger 3) and DRA (Down Regulated in Adenoma) work in conjunction to mediate electroneutral NaCl absorption. Electrogenic mode of Na+ absorption occurs in the distal part of colon via ENaC (Epithelial sodium channel). Intracellular Na+ gradient essential for sodium dependent transport processes is generated by the action of Na+/K+-ATPase present at the basolateral membrane. Cl− secretion across the membrane is facilitated by apical Cl− channel CFTR (cystic fibrosis transmembrane conductance regulator). Basolateral NKCC1 (Na+/K+/2Cl− cotransport system) is involved in uptake of Cl− from the serosal side. K+ taken up by NKCC1 and Na+/K+-ATPase is recycled back to the basolateral side by K+ channels localized to the basolateral membrane. Predominant mechanism of diarrhea in IBD involves impairment of electroneutral NaCl absorption accompanied with dysfunctional ENaC and Na+/K+-ATPase, with very little role if any played by anion secretion. Negative sign indicates the downregulation in function and/or expression of NHE3, DRA, ENaC and Na+/K+-ATPase in IBD. The mucus layers serves as a barrier and prevents the direct contact of gut microbes with the underlying epithelium. Adjacent intestinal epithelial cells are sealed together via an intricate network of junctional proteins including the tight junction (TJ) proteins (claudins, occludin, JAM and ZO-1), adherens junction (AJ, E-cadherin) and desmosomes. The optimal expression and function of tight and adherens junction proteins regulate the paracellular flux under physiological conditions. Negative sign indicates the downregulation in function and/or expression of TJ and AJ proteins in IBD. Breakdown of barrier function in IBD results in diarrhea via leak-flux mechanism. As summarized in the review, understanding of the mechanisms underlying loss of barrier function and defective ion absorption in IBD is essential for development of better treatment strategies for IBD and associated diarrhea.
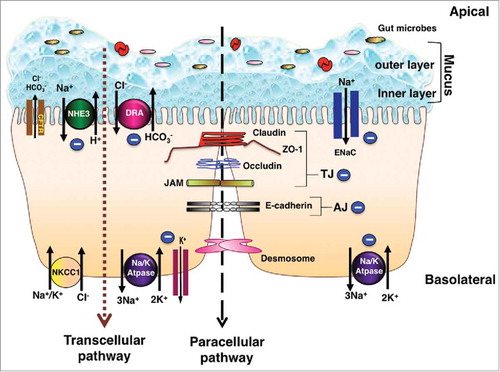
Table 1. Modulation of Ion transporters and channels involved in sodium and chloride absorption in IBD Patients.
Table 2. Alterations in Tight junction proteins in IBD Patients.
