Figures & data
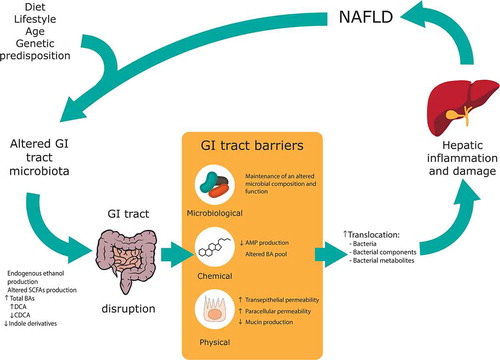
Figure 1. Structure of microbiological, chemical, physical and immunological barriers in the intestine. The microbiological barrier resides in the intestinal lumen, over and inside the mucus. It is composed of intestinal microbiota including bacteria, fungi, archaea and viruses. The mucus layer forms part of the physical barrier (coating with a single layer the small intestine and with a double layer the large intestine), in which AMP, BA and SIgA are secreted and they act as chemical barriers. The mucus covers the intestinal epithelial cells, which are also considered part of the physical barrier. Moreover, these cells are tightly sealed by TJs (claudins, occludin, ZOs), JAM-A and by AJs (E-cadherin) controlling the paracellular permeability. Scattered throughout the epithelium and lamina propria, innate immune cells (i.e. macrophages, dendritic cells and lymphoid cells) and adaptive immune cells (i.e. T and B cells) reside. In the lamina propria of the gut mucosa, endothelial cells tightly sealed by claudin, occludin, JAM-A and VE-cadherin proteins form a gut vascular barrier.; AJs: adherens junctions, AMP: antimicrobial peptides, BA: bile acids, SIgA: Immunoglobulin A, JAM-A: TJs-associated adhesion molecules, TJs: tight junctions, VE-cadherin: vascular-endothelial cadherin, ZOs: zonula occludens
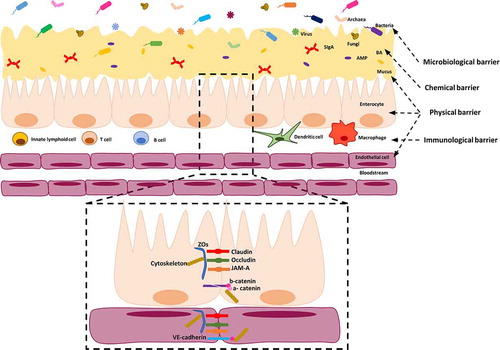
Figure 2. Alterations in gastrointestinal (GI) tract barriers associated with nonalcoholic fatty liver disease (NAFLD) pathogenesis. An altered GI tract microbiota due to diet, lifestyle, age and genetic predisposition can lead to an altered pool of metabolites along the GI tract. An altered microbiota and metabolite composition can lead to GI tract barriers disruption, with a special focus in this review to the microbiological, chemical and physical barriers. The increase in gut permeability leads to an incremented translocation of bacteria, bacterial components and bacterial metabolites to the portal system; which ultimately cause hepatic inflammation and damage and, hence, contributing to NAFLD pathogenesis. SCFA: Short-chain fatty acid, BA: Bile acid, DCA: Deoxycholic acid, CDCA: Chenodeoxycholic acid; AMP: Antimicrobial peptides