Figures & data
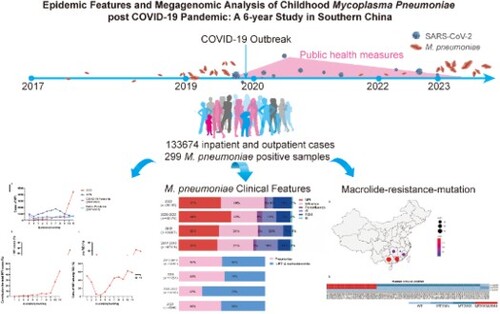
Figure 1. Data handling process and analysis diagram. There were 1,33,674 patients were included for data analysis. Additionally, macrolide-resistance-mutation characteristics of Mycoplasma pneumoniae were analysed based on samples from 299 patients.
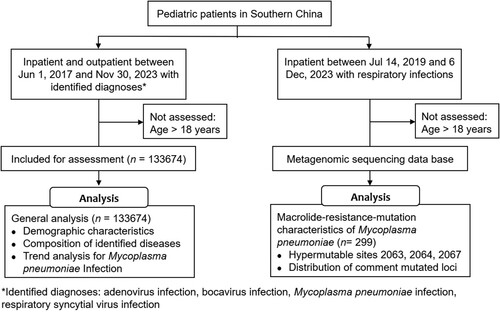
Table 1. Demographic characteristics of paediatric patients with common respiratory infectious diseases.
Table 2. Monthly average cases and change proportion of common respiratory infectious diseases in paediatric patients during observation.
Figure 2. Changes in case distribution for common respiratory infectious diseases before and after the COVID-19 pandemic in paediatric patients. Outbreaks of MPI were noted in 2019 and 2023, while the decrease of MPI was associated with enhanced public health measures during COVID-19 pandemic (timeframes marked with shadow). Abbreviations: AI, adenovirus infection; BI, bocavirus infection; MPI, Mycoplasma pneumoniae infection; and RSVI, respiratory syncytial virus infection.
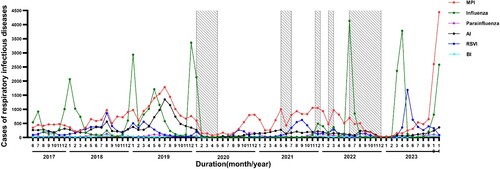
Figure 3. Case distribution of MPI in observation duration. The peak cases of MPI in 2023 was twice more than that in the outbreak in 2019 (A). The cases of MPI were accumulated specifically in October and November 2023 (B), which contributed around 60.0% of cases among RID (C). Abbreviations: MPI, Mycoplasma pneumoniae infection and RID, respiratory infectious diseases.
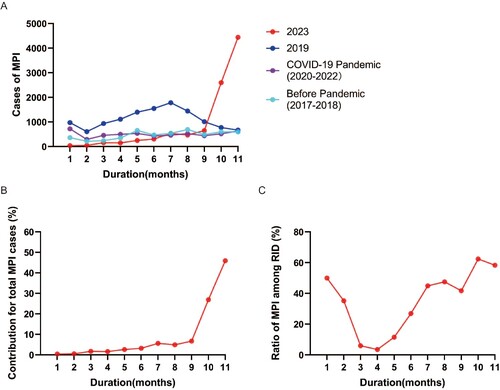
Figure 4. Disease spectrum of paediatric common respiratory infectious disease (RID) and the clinical manifestation of MPI before and after the COVID-19 pandemic. The annual proportion of MPI was stable between 34.0% and 46.0% among RID from 2017 to 2023 (A). The cases of MP-associated pneumoniae were similar between the outbreaks in 2023 and 2019, while a remarkable decrease was observed with enhanced public health measures during the COVID-19 pandemic from 2020 to 2022 (B). Abbreviations: AI, adenovirus infection; BI, bocavirus infection; MPI, Mycoplasma pneumoniae infection; RSVI, respiratory syncytial virus infection; and URTI, upper respiratory tract infection.
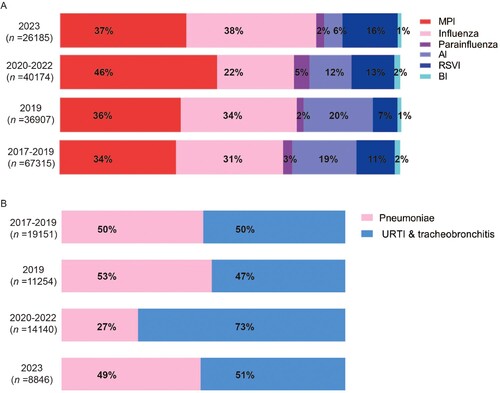
Table 3. Monthly average cases and change proportion of paediatric patients with Mycoplasma pneumoniae infection.
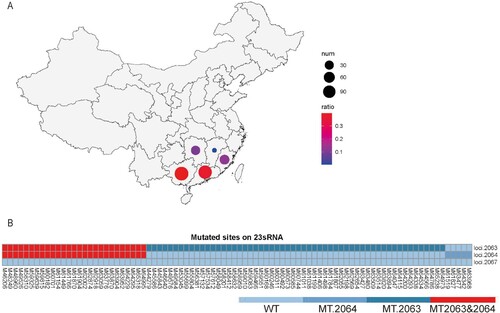
Figure 5. Macrolide-resistance-mutation characterizations of MP in the recent prevalence in Southern China. Positive MP sequences were identified in 299 samples from five provinces in Southern China (A), and mutations were detected in macrolide-resistance hypervariable sites including loci 2063 and 2064 (B).
Supplemental Material
Download MS Word (415.6 KB)Data availability statement
De-identified participant data supporting the conclusions of the current study are available upon publication to researchers by email to the corresponding author on reasonable request for research.