Figures & data
Figure 1. Illustration (A) showing two foci of Grade 1 invasive ductal carcinomas (4 cm apart) in the right breast and two foci of Grade 1 invasive ductal carcinomas (5 cm apart) in the inferior-central and inferior part of the left breast. Bilateral breast MRI with contrast (B) showing an irregular enhancing lesion in the upper outer quadrant measuring 12 × 8 × 13 mm and a second malignancy, measuring 9 × 6 × 11 mm in the upper medial aspect of the right breast at the same level as lesion 1. The left breast (C) shows a 7 mm irregular enhancing lesion at the 6 o’clock position and (D) a second lesion measuring 5 mm located inferolateral to this.
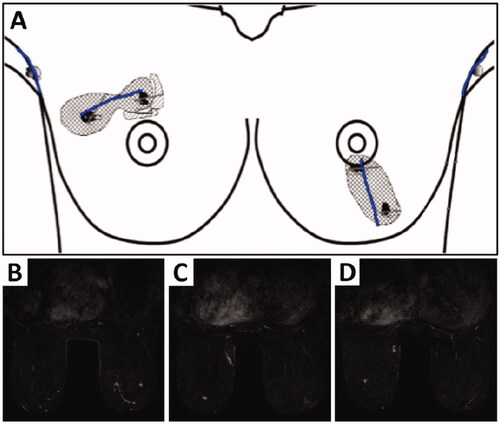
Figure 2. Intraoperative surgical markings on the left index breast outlining a round neoareola (shaded green, marked G) of the inferolaterally-based Grisotti flap and the location of the inferomedial secondary pedicle with its overlying skin (shaded red, marked P) prior to de-epithelialisation. The Wise pattern (deep black markings) is superimposed on these markings.
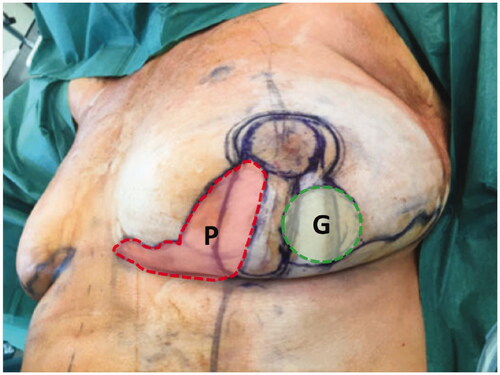
Figure 3. (A) Following central and inferior segment excision on left breast, a circular skin paddle (neo-areola) on the laterally-based Grisotti flap is marked. The shaded zone is the part of the Grisotti flap that will be de-epithelialised. The part of the breast medial to the inferior segmental defect inside the Wise pattern markings will be totally de-epithelialised and constituted the secondary pedicle. (B) The inferomedially-based secondary pedicle (underneath the scissors) is transposed and advanced into the deep part of the central defect which is about to be buried by suturing it to the pectoral fascia. (C) After fixation of secondary pedicle into the central defect, the Grisotti flap is advanced into the defect on top of/superficial to the secondary pedicle. (D) The Wise pattern ‘wings’ are being prepared to be approximated superficially to the de-epithelialised part of the Grisotti flap. (E) Both flaps (Grisotti & secondary pedicle), which are designed to fill central and inferior cavity defect, are now in place prior to closure. (F) Completion of the right superomedial pedicle Wise pattern breast reduction and breast-conserving surgery on the left breast, showing reasonable on-table symmetry.
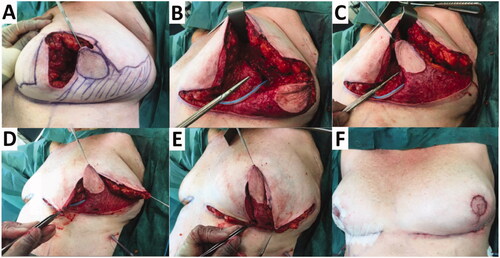
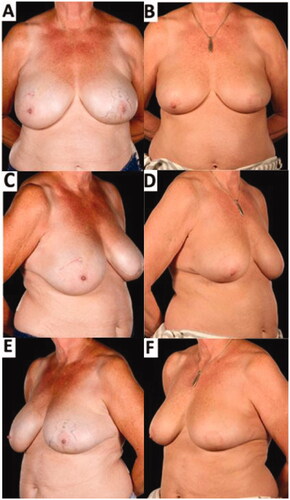
Figure 4. Pre-operative (A,C,E) and 8-months post-operative (B,D,F) appearances of a 61-year-old patient who underwent breast-conserving surgery comprising a redo-wide local excision (central and inferior segmental resection including the NAC) reconstructed with a laterally-based Grisotti flap and an inferiorly-based secondary dermoglandular pedicle and simultaneous contralateral symmetrising breast reduction – 6 months after completion of adjuvant radiotherapy. The improved breast symmetry was made possible by the complex oncoplastic techniques. The patient declined formal nipple reconstruction preferring intermittent use of a prosthetic nipple. There was no residual visible skin reaction from the radiotherapy treatment.