Figures & data
Figure 1. (A) The defect after debridement. (B) Flap design. The blue dot marks the perforator identified with the handled doppler probe.
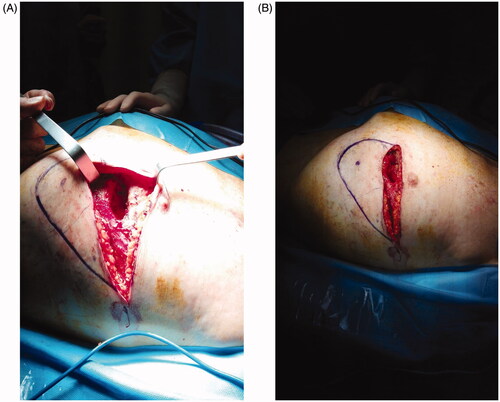
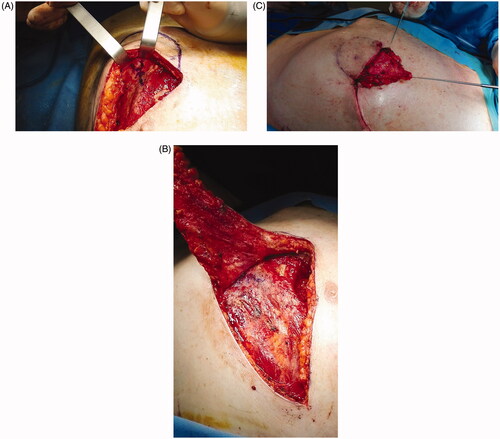
Figure 2. Flap raising. After perforator identification, incision of the lower margin and flap raising (A). (B) De-epithelialization and transposition of the proximal portion of the flap. (C) The wound 1 week post-op.