Figures & data
Figure 1. Surgical technique. (A) Recipient site after radical resection of basal cell carcinoma. (B) Preoperative marking at the donor site. Note the marking of the harvested cartilage (solid line) which were approximately 3–5 mm in height and 3–5 mm in length and the skin (dashed line). (C) Cartilage wings in place, secured in subcutaneous pockets parallel to the alar rim with dissolvable sutures. (D) Composite graft in place.
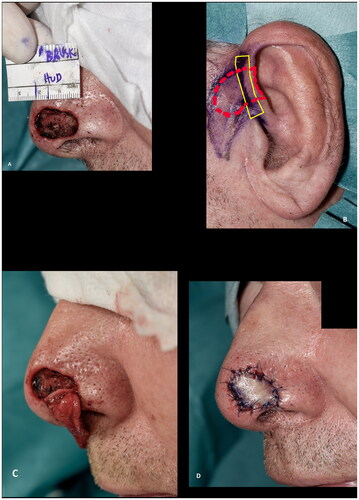
Figure 2. (A,B) A defect after radical resection of basal cell carcinoma involving the alar rim reconstructed with a composite graft. (C) Epidermolysis eleven days after surgery. (D) The graft at two months follow up. (E) Despite the partial graft loss and alar retraction at three months follow up the outcome was rated as acceptable.
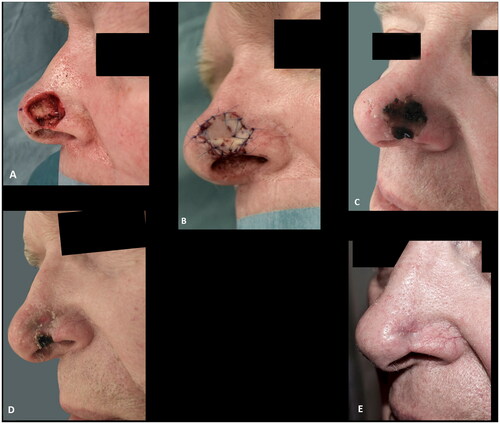
Figure 3. (A) 81-years-old female with a basal cell carcinoma causing alar retraction prior to surgery. (B) The large full thickness defect after radical resection of basal cell carcinoma involving the whole alar subunit and part of the lower nasal sidewall. (C) The patient declined the offered paramedian forehead flap and was subsequently reconstructed with a composite graft. A suture was placed in the center of the graft to imitate the alar sulcus, which might have added to the poor graft take, as partial graft loss occurred, despite the large wound bed, as evident on images (B–G). (H,I) The remaining healed graft, as seen eight months postoperative, provided stability for an exoprosthesis and for skin-coloured surgical tape (Micropore™) that the patient considered to be more convenient to use. The patient declined revision surgery. This outcome was rated as poor.

Figure 4. (A,B) A superficial defect, 2 mm from the alar rim, reconstructed with a composite graft to prevent alar retraction. (C) The composite graft at the first change of dressing after six days. (D–F) The results at five months follow-up, showing a good result with intact contour of the alar rim. Additionally, a good result at the donor site at the crus of helix.
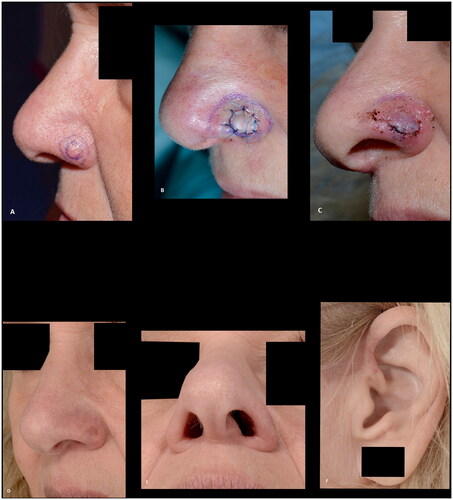
Figure 5. (A,B) A basal cell carcinoma, close to the alar margin, reconstructed with a composite graft maintaining the contour of the alar margin. The outcome was rated as good. This patient, however, experienced discomfort caused by the cartilage protrusion (arrow) and revision surgery was performed.
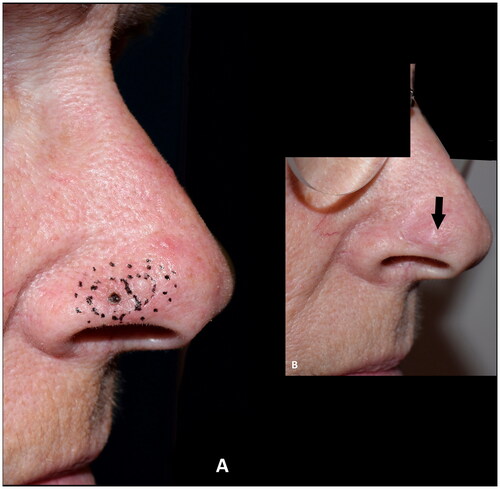
Figure 6. (A) Resection of basal cell carcinoma at the right alar rim, which was left to heal by secondary intention. (B) Shrinkage and collapse of the nostril led to nasal obstruction, which was evident at four months follow up. Note the shortened height of the ala in comparison to the contralateral ala (yellow arrows). (C–F) Revision surgery with a composite graft from the posterior surface of the ear was performed nine months after the defect was left to heal secondarily, successfully alleviating the nasal obstruction. Note the cautious cautery to the wound bed and the wide cartilage wings needed to stabilize the alar I. (G) An excellent functional outcome was observed three months later. (H,I) At twenty-two months follow up the functional outcome was still excellent, and the discoloration had subsided and donor site had healed well. The outcome was rated as good.
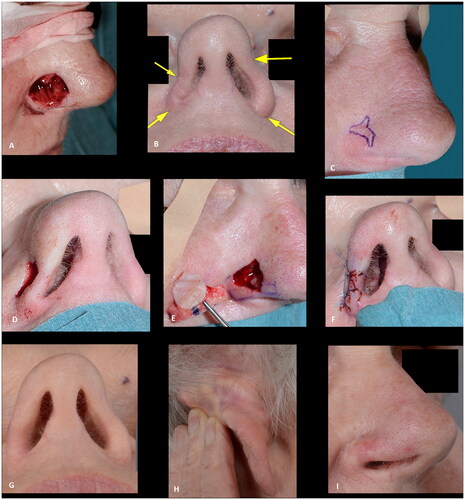
Figure 7. (A) A pyogenic granuloma involving the nasal tip and soft triangle. (B) The superficial defect two days later (after the final histology report was clear of the granuloma). (C) The result, three months after closure of the defect with a full-thickness skin graft, showing an unacceptable alar retraction at the soft triangle. (D–E) Nine months after the first reconstruction, revision surgery was performed with a composite graft correcting the alar retraction with a more acceptable result after three months. Note the excision of the skin above the full thickness defect, allowing for a well vascularized wound bed for graft take. The outcome was rated as acceptable due to alar retraction.
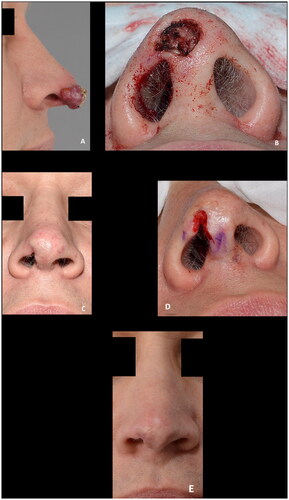
Table 1. Demographic, procedure, and postoperative characteristics of 18 patients undergoing composite grafts for nasal reconstruction.
Figure 8. (A–D) A large superficial defect with a smaller full thickness defect measuring 4 × 12 mm, providing a well-vascularized recipient site for graft take. Note the nasal airway secured to maintain the airway, eliminate dead space, immobilize the graft and to preserve the shape of the nasal ala while the graft heals. (E) The result at the first dressing change seven days postoperative. (F–H) Fourteen months postoperative showing results rated as good. Courtesy of consultant, plastic and reconstructive surgeon Jais Oliver Berg, Dep. of Plastic Surgery, Herlev and Gentofte Hospital, Denmark.
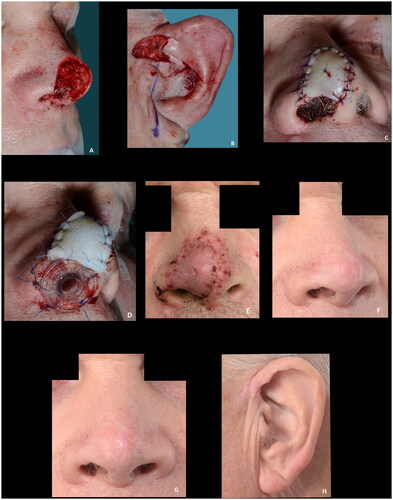
Figure 9. (A,B) Intraoperative view of the full thickness defect and the composite graft. (C–E) Composite graft at seven, thirteen and sixteen days postoperatively. (F) The result six weeks postoperative after secondary healing. The patient declined further reconstruction. The outcome was rated as poor.

