Figures & data
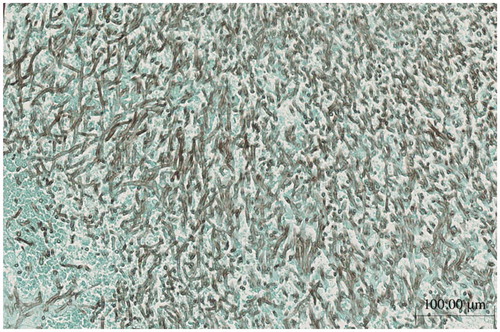
Figure 1. (A) The fat-suppression T1-weighted MRI showing subcutaneous thickening and partial vascular flow void signal that correspond with left temporal artery; arrow. (B) Left temporal artery biopsy (TAB) revealed the intimal fibrous thickening, small rupture and fibrotic change of internal elastic lamina (left panel; Elastica-Masson staining, white arrows). No apparent inflammatory cell infiltration or giant cell (right panel; Hematoxylin and Eosin staining).
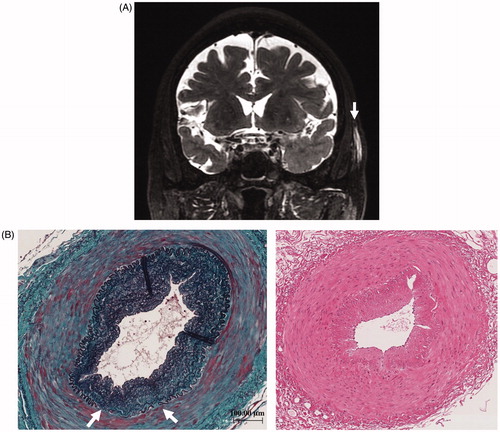
Figure 2. (A) Chest CT; at the onset of severe pneumonitis caused by Pseudomonas aeruginosa. (B) Chest CT; inflammatory cavitary lesion was remained in right upper lobe after sepsis treatment. (C) Chest CT; obvious cavitary lung lesion in the right upper lobe.
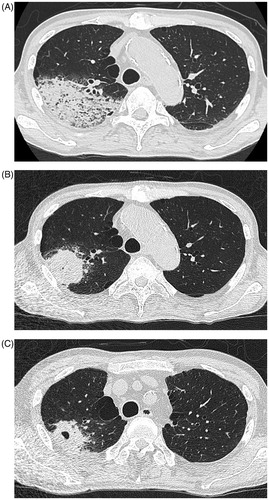
Figure 3. Contrast enhanced T1-weighted MRI showing enhancement of the dura beneath the left temporal lobe, compatible to hypertrophic pachymeningitis.
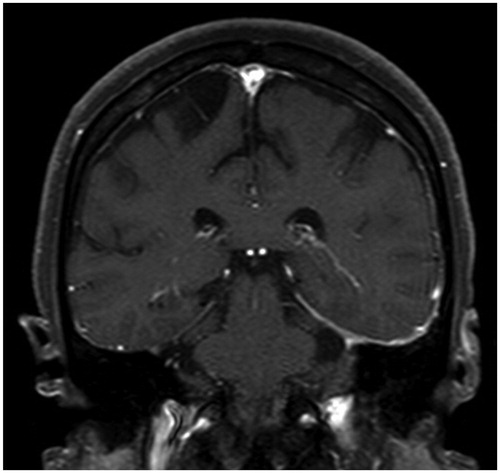
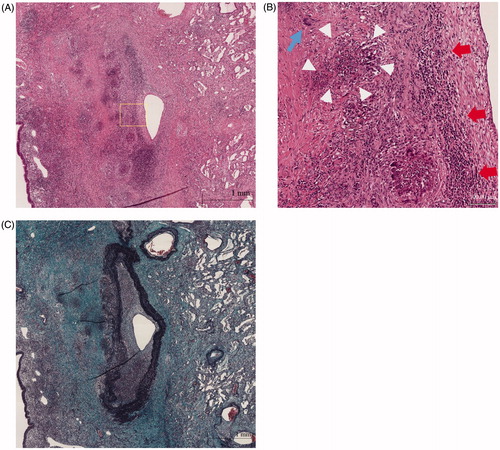
Figure 4. (A) Histopathology of lung lesion in right upper lobe (Hematoxylin and Eosin staining). (B) Higher power field of (A); diffuse infiltration of lymphocytes and necrotizing vasculitis with bronchocentric granulomatosis. Giant cell (blue arrow), inflammatory cells (red arrows), fibrinoid degeneration (circle of white arrowheads). (C) Histopathology of lung lesion in right upper lobe (Elastica Masson staining).