Figures & data
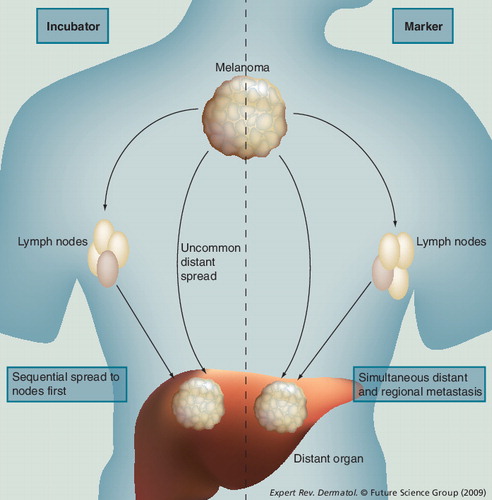
The incubator hypothesis: primary melanoma spreads first to regional draining nodes and only subsequently to distant sites. The marker hypothesis: spread occurs simultaneously to nodal and distant sites.
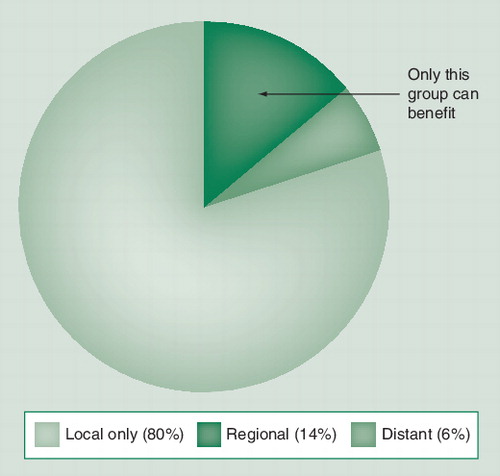
The majority of cases (80%) are limited to the primary site, while a smaller fraction (6%) have disease already beyond the regional nodes. Only those with nodal disease but not systemic disease (14%) will be cured by early nodal excision.
Subgroup 1: patients with positive sentinel lymph node (SLN). Subgroup 2: those with positive SLN or false-negative SLN. Subgroup 3: those with nodal recurrence in the wide excision-alone arm.
Subgroup 4: those with false-negative SLN.
Redrawn with permission from Citation[7] © 2006 Massachusetts Medical Society. All rights reserved.
![Figure 3. Melanoma-specific survival in the Multicenter Selective Lymphadenectomy Trial clinical trial.Subgroup 1: patients with positive sentinel lymph node (SLN). Subgroup 2: those with positive SLN or false-negative SLN. Subgroup 3: those with nodal recurrence in the wide excision-alone arm.Subgroup 4: those with false-negative SLN.Redrawn with permission from Citation[7] © 2006 Massachusetts Medical Society. All rights reserved.](/cms/asset/463f8e8e-77bb-43fe-898a-c486ea2f0c95/ierg_a_11208297_f0003_b.jpg)