Figures & data
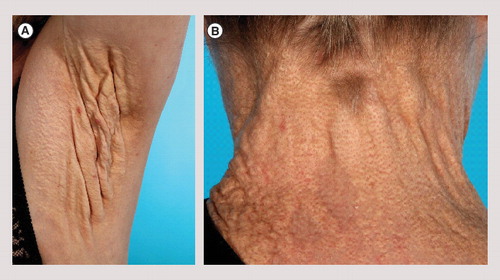
(A) Axillary plaque with severe loss of elasticity in a 56-year-old woman. (B) Late skin symptoms showing coalesced yellow papules forming a plaque surrounding the neck in a 56-year-old woman.
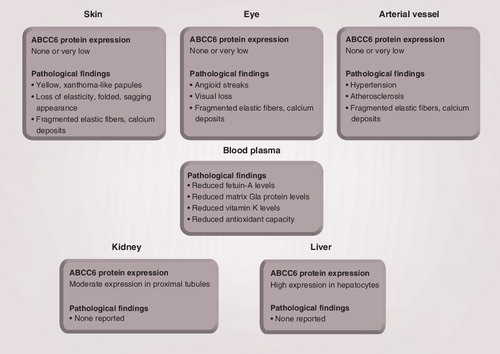
Pseudoxanthoma elasticum-affected tissues like the skin, the eye and the arterial vessel appear devoid of ABCC6 protein. Moderate ABCC6 expression is detected in the kidney, whereas ABCC6 is highly expressed in the liver. No pathological findings have been reported in the kidney and liver of pseudoxanthoma elasticum patients.
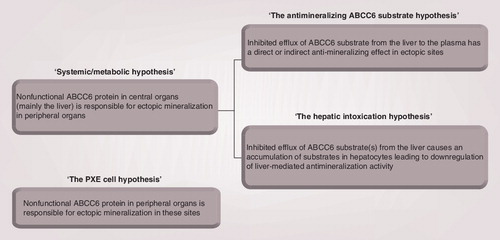
The systemic/metabolic hypothesis of PXE pathogenesis can be divided into two subcategories. ‘The antimineralizing ABCC6 substrate hypothesis’ states that the ABCC6 substrate has antimineralizing properties, and that PXE-related ectopic mineralization is caused by a diminished secretion of this substance from the liver. According to ‘the hepatic intoxication hypothesis’, PXE ectopic mineralization is due to hepatic accumulation of ABCC6 substrate(s) that leads to gene-regulatory changes of hepatic proteins involved in calcification. ‘The PXE cell hypothesis’ states that nonfunctional ABCC6 protein in PXE-affected tissues is the cause of ectopic mineralization in these sites.
PXE: Pseudoxanthoma elasticum.