Figures & data
Table 1 DAH – the key points
Figure 1 Local pulmonary administration of FVIIa into the airways ensures that the drug reaches its alveolar receptor TF. However, most importantly, taking into account the separation between the two compartments the “air side” and the “systemic side”, there will not be systemic adverse effects in as much as the alveolo-capillary membrane does not allow the transmembranous passage of FVIIa, when inhaled. FVIIa does not pass through the alveolo-capillary membrane either from the (A) alveolus or (B) the blood side.
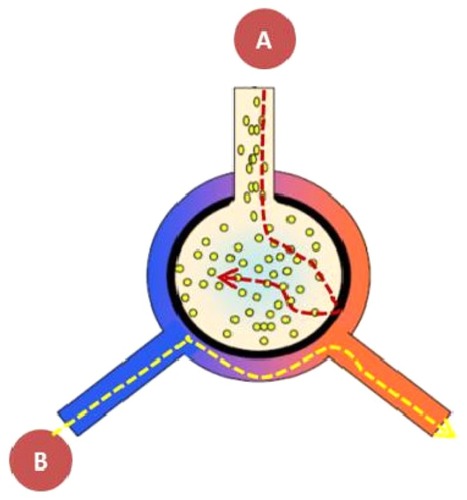
Figure 2 The DAH syndrome is the common denominator of multiple diseases and conditions. DAH is the general alveolar response to multiple underlying diseases and conditions. The syndrome DAH manifests itself in three subsets: the acute catastrophic DAH, the chronic DAH and finally as the instant blast lung injury. The acute DAH has been treated with local intrapulmonary FVIIa administration. The two other subsets could potentially also be treated from the air side, an intervention which remains to be shown.
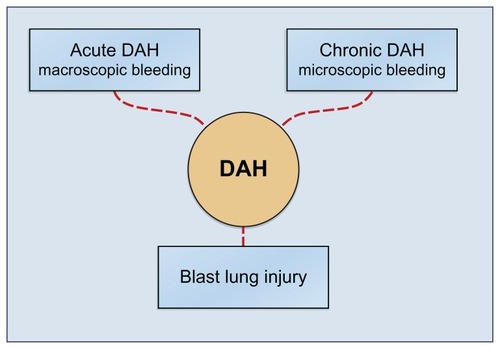
Table 2 Overview of diseasesyndromes and other causes leading to DAH and the classical options of treatment
Figure 3 The diagnostic algorithm for DAH, BOOP and ARDS. The clinical signs and symptoms of DAH, ALI/ARDS and BOOP are identical, ie, chest film with confluent opacities, acute pulmonary insufficiency with reduced O2 transport capacity. It is imperative to separate between the specific diagnoses of each of these conditions, in as much as they all have a high mortality; it is of utmost importance to diagnose correctly because the specific therapies are different. The simple algorithmic separation is based on progressively hemorrhagic aliquot of a series of BALF’s either macroscopically which denote a severe DAH syndrome or measurements of an increased hemoglobin concentration in the BALF which corresponds to a slow bleeding DAH like in IPH. Provided there is no bloody return at the BALF the DAH diagnosis is excluded. The remaining two conditions are separated by a simple flow-cytometry on the BALF, where the BOOP is characterized by abundant inflammatory cells, and the ARDS diagnosis is based on a BALF without inflammatory cells or bloody return.
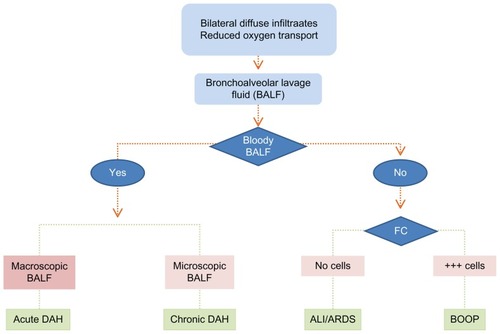
Table 3 Overview of BLI – a dynamic conditionCitation23
Table 4 After a major blast the three phases have their own distinct problemsCitation24–Citation26
Table 5 Diffuse alveolar hemorrhage – the treatment paradigm
Figure 4 It is essential to separate cause and the effect of DAH. It is important to separate the treatment of multiple underlying causes of DAH from the common complicating denominator DAH syndrome, because the latter is simply treated with local pulmonary FVIIa.
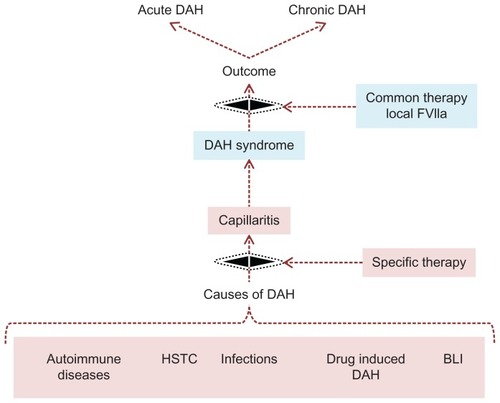
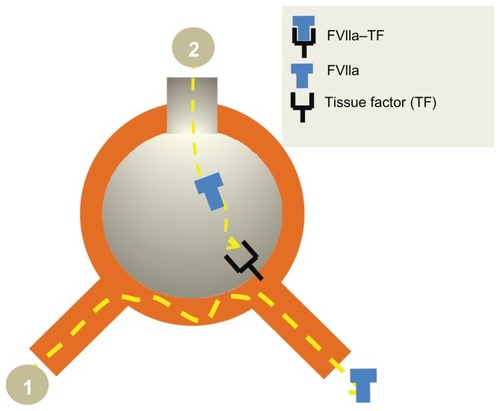
Figure 5 Rationale for local pulmonary treatment of DAH with FVIIa. Intravenous rFVIIa does not reach the alveoli (1) in contrast to the airway route (2) where a direct access to the receptor TF is obtained. The TF-FVIIa complex activates coagulation factor IX and X. Finally the activated TF-FVIIa complex induces a perfect “balanced” hemostasis ie, sufficient fibrin deposition without interference with the oxygen transport. The TFPI are constitutively expressed in the airspace in inflammatory conditions, secondary to alveolar inflammation. The TFPI is usually of less importance as compared to the procoagulatory factors. However, this might be the explanation for the balanced hemostasis.