Figures & data
Figure 1 Principle of the motility tracking system for evaluation of gut motility.
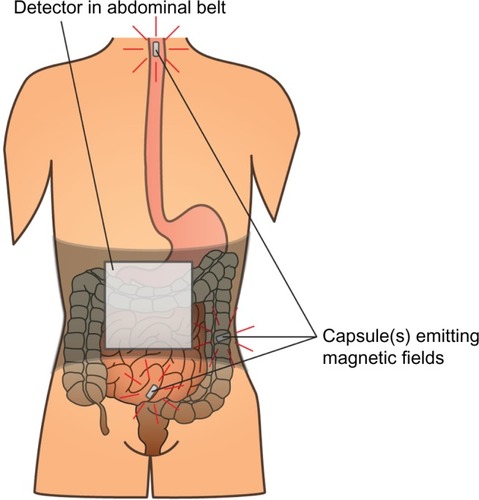
Figure 2 Schematic representation of the Ussing chamber measuring gut secretion.
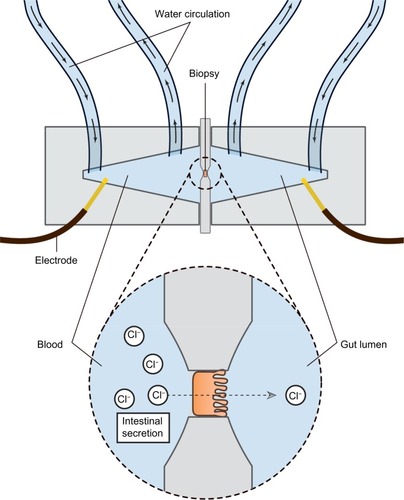
Figure 3 The FLIP probe.
Abbreviation: FLIP, functional lumen imaging probe technique.
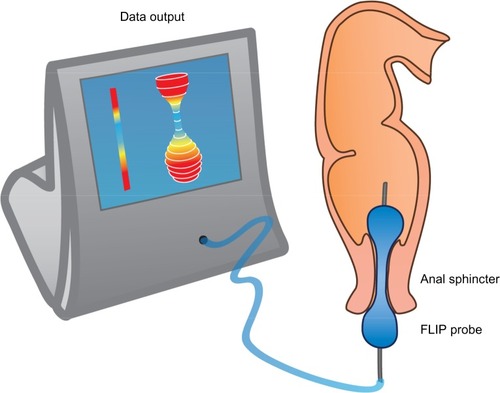
Table 1 Underlying mechanisms, symptoms, and the potential effects of PAMORAs and laxatives, respectively
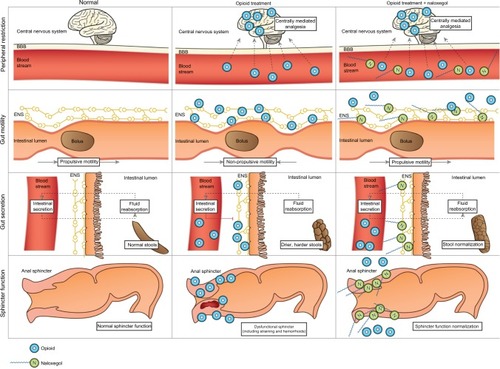
Figure 4 Pharmacological principle of naloxegol under normal conditions (left column), during opioid treatment (middle) and opioid and naloxegol treatment (right).
Abbreviations: ENS, enteric nervous system; BBB, blood–brain barrier.