Figures & data
Figure 1 Crude incidence proportion of bleeding events during index admission*.
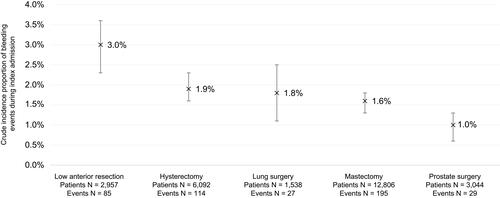
Table 1 Patient Characteristics*
Table 2 Characteristics of Index Admission and Surgery*
Figure 2 Adjusted association of bleeding events with post-procedural hospital length of stay*.
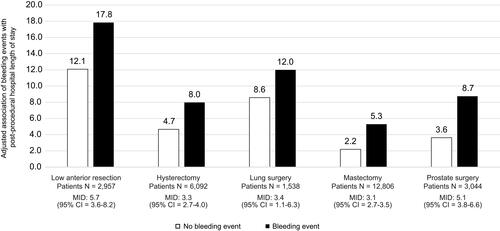
Figure 3 Adjusted association of bleeding events with post-procedural days spent in critical care*.

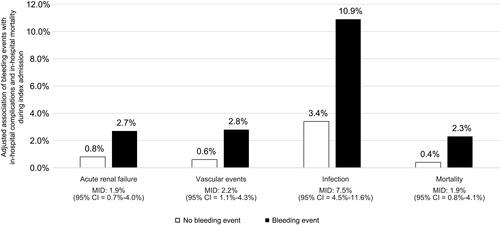
Figure 4 Adjusted association of bleeding events with in-hospital sequelae and in-hospital mortality during index admission*.