Figures & data
Table 1 Treatment Efficacy: Odds Ratio for Response Rate
Table 2 Simplified Dosing Table
Table 3 Resource Use Associated with Infusion of IV Iron Formulations
Table 4 Pack Contents and Pack Costs of IV Iron Formulations
Figure 1 Number needed to treat to bring achieve one additional responder with ferric carboxymaltose versus other therapy options. Number needed to treat was expressed as the number of patients who would need to be treated to with ferric carboxymaltose instead of the comparator in order achieve one additional responder. Number needed to treat values are conventionally rounded up to the next integer value. Only the difference between the efficacy of FCM and oral iron was based on a statistically significant difference in the model input.
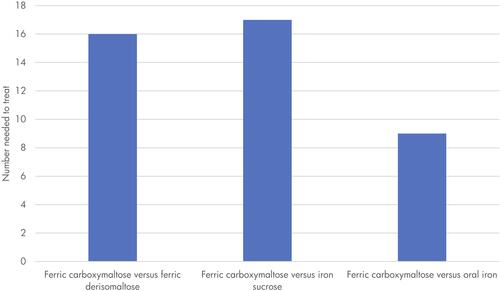
Table 5 Results of the Base Case Modelling Analysis
Figure 2 Scatterplot of the base case results. GBP, 2020 pounds sterling. Response was defined as a patient who achieved normalisation of haemoglobin levels or an increase in haemoglobin of ≥2 g/dL.
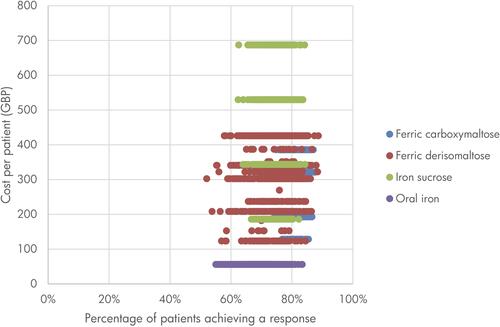
Table 6 Scenario Analysis Results
Table 7 Sensitivity Analysis Results
